Secondary repair of severe chronic fourth-degree perineal tear due to obstetric trauma
ABSTRACT
Obstetric injury is the commonest cause of anal incontinence. We report a case of anal incontinence as a result of severe chronic fourth-degree perineal tear secondary to birthing with complete disruption of the perineum.The outcome of anterior sphincter repair following obstetric trauma is good but long-term follow-up is required because of the underlying complexity of obstetric injury. As prevention is not always possible, immediate recognition and adequate primary treatment is of importance.
INTRODUCTION
Obstetric injury is the most common cause of sphincter injury and pelvic floor failure resulting in lack of bowel control. The pudendal nerve may be damaged during the course of prolonged vaginal delivery consequent to stretching . 4 to 6% of women who have vaginal deliveries will suff er from faecal incontinence . A third/fourth-degree tear (involving the anal sphincter complex) occurs in 0.5–2%. Eighty five per cent will have a persistent defect of the sphincter despite the immediate (primary) repair by the obstetrician . Conservative treatment (diet/medical manipulation, biofeedback and pelvic floor exercises) can be successful. Secondary repair is usually off ered to patients with gross faecal incontinence . The outcome depends on the extent of the anal sphincter damage and associated neurological injury .
Risk Factors for Obstetric Anal Sphincter Injuries
Based on meta-analysis of data from 22 studies (the strongest risk factors for OASIS included
- forceps delivery
- vacuum-assisted delivery
- increased fetal birth weight
- Midline episiotomy combined with forceps delivery substantially increases the risk of third-degree fourth-degree laceration (8). The risk of anal sphincter trauma with operative delivery and episiotomy is increased in primigravid women and multigravid women (21).
Based on the same meta-analysis data, other risk factors for OASIS include
- primiparity
- Asian ethnicity
- labor induction
- labor augmentation
- epidural anesthesia
- persistent occiput posterior position
CASE REPORT:
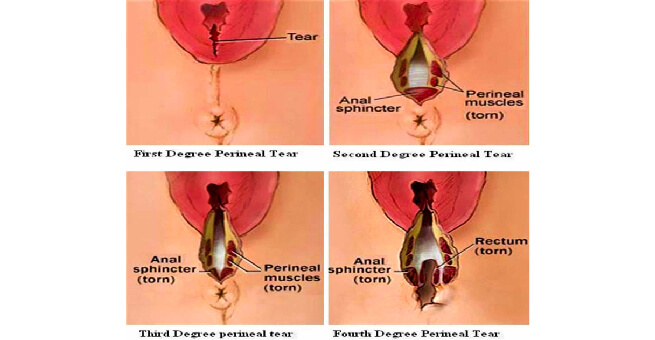
A 30 yrs female presented to the OPD with complaint of anal incontinence since 1 year. It started 5 days post delivery with progressive loss of continence to flatus and faeces.Obstetric history revealed that she delivered large baby of weight 4 kg in 2022 . There was no history of prolonged labour or instrumental delivery . complete fourth degree perinea tear was diagnosed at the time of delivery and repaired immediately. But she presented with wound dehiscence on 4 th post natal day . Again repair was done . Following which she started having ANAL incontinence .
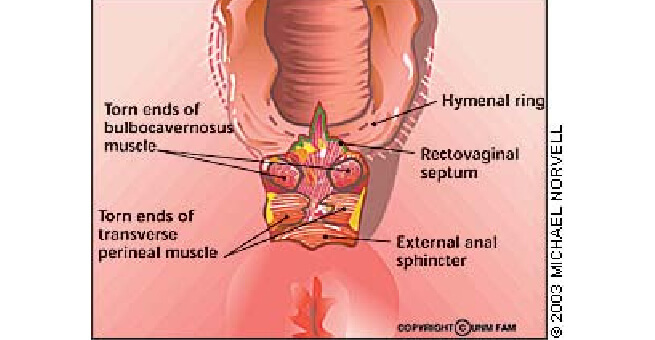
Physical examination revealed a patulous anus immediately adjacent to the posterior forchette of the vagina indicating a poor internal sphincter function . Loss of corrugated appearance anterior to anal orifice.Dimpling of skin noted lateral to anal orifice on both sides .She had a lax external sphincter tone on voluntary squeezing .Anal wall defect of 1.5 cms noted . A preoperative diagnosis of a fourth-degree perineal tear involving the internal anal sphincter (IAS) and external anal sphincter (EAS) was made and she consented to a perineal repair .
Table 1
Classification of perineal tear [4]
|
First degree |
Injury to perineal skin |
|---|---|
|
Second degree |
Injury to perineum involving perineal muscles but not involving the anal sphincters |
|
Third degree |
Injury to perineum involving the anal sphincter complex:3a: <50% of ext anal sphincter thickness3b: >50% EAS thickness3c: both EAS and IAS involved |
|
Fourth degree |
Involves anal sphincter complex (EAS and IAS) and anorectal |
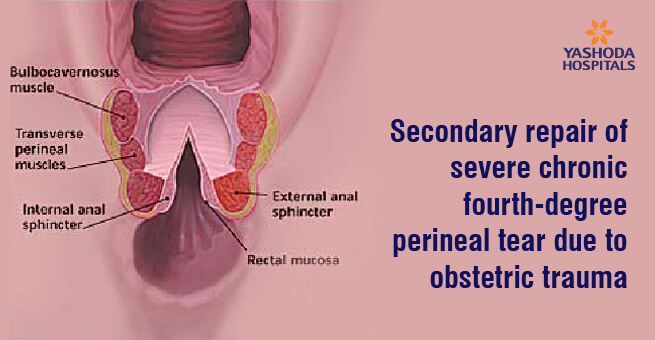
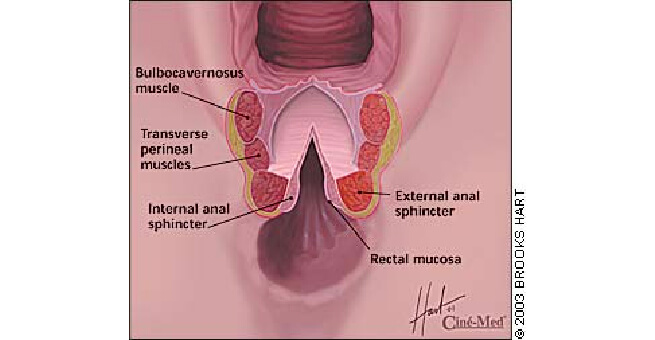
procedure was performed under spinal anaesthesia with preoperative bowel preparation and prophylactic antibiotics . The woman was placed in the lithotomy position.A transverse incision given at the junction of rectal anal mucosa , and incision extended up in the midline of posterior vaginal wall . With careful sharp dissection rectal wall has been separated from the posterior vaginal wall . External anal sphincter identified and held with Alli’s clamps.Defect in the anal mucosa sutured intermittently with 3 0 PDS .Internal anal sphincter identified and sutured intermittently with 3 0 PDS .External anal sphincter approximated by overlapping technique with 2 0 PDS. Rectovaginal fascia tightened.Superficial Transverse perineal muscles and bulbocavernosus muscle anchored to perineal body Vaginal mucosa sutured continuously with 2 0 PDS . Perineal skin closed subcuticularly.
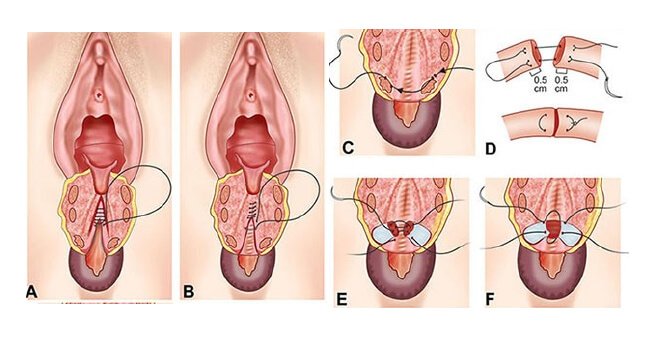
Fourth-degree perineal tear
A – suturing of rectal mucosa
B – suturing of internal sphincter
C ,D,E,F – suturing of external anal sphincter
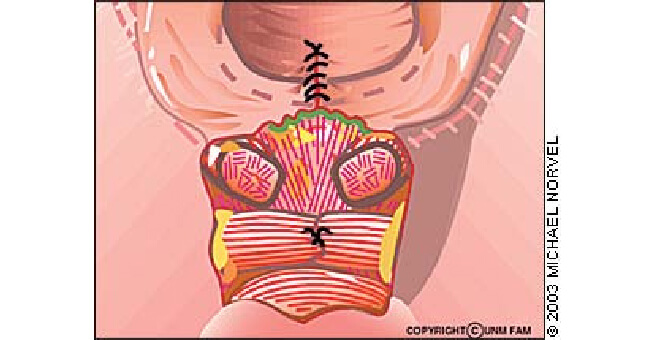
Suturing of transverse perineal muscles
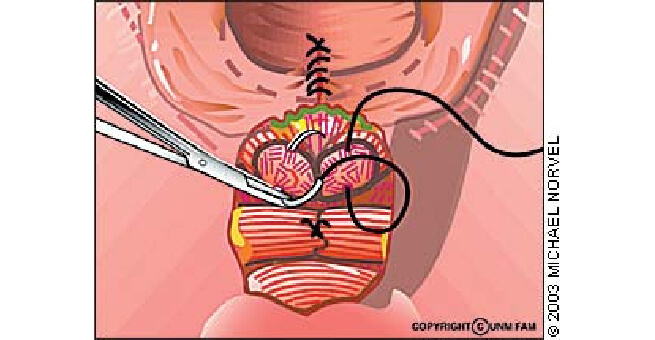
Suturing of bulbocavernosus muscle
Postoperatively patient was allowed liquid diet and semisolid diet followed by soft diet. Perineal care with sitz bath given.
Follow up
Physiotherapy
Sitz bath twice daily for 2 weeks
Laxatives for 4 weeks
Abstinence for 8 weeks
Endoanal ultrasound after 3 months
DISCUSSION
Primary repair is ideal as successful primary sphincteroplasty substantially improves quality of life and reduces overall cost of treatment . In a resourced area, endoanal ultrasound will localize the injury site and size the extent of sphincter damage prior to a secondary repair . management is usually off ered to a patient an underlying correctable abnormality and gross faecal continence . Improvement inthe functional length of the sphincter corresponded to a successful outcome . Long-term follow-up is thus required.
Prevention Strategies
- warm compresses during second stage
Role of Episiotomy
- Existing evidence supports restrictive episiotomy vs routine
- Some evidence that mediolateral episiotomy is superior to midline episiotomy,if necessary, with lower rates of OASIS


 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

