Cutaneous Implantation Submandibular Pleomorphic Adenoma: An Unusual Presentation
Introduction
Salivary gland neoplasms are uncommon but generate considerable interest because of their remarkable variation in clinical presentation, histologic appearance and behavior. They may arise in the major salivary glands (parotid, submandibular, and sublingual) or the so-called minor salivary glands, which are small, predominantly mucus-secreting glands located beneath the mucosal lining of the upper aerodigestive tract.
Salivary gland tumors comprising less than 3% of all neoplasia of the head and neck region.
- Pleomorphic Adenoma, also known as the benign mixed tumor is the most common tumor of the salivary gland accounting for 60-80% of the benign variety. The submandibular gland is involved in only 5% to 10% of the salivary gland tumors, and Pleomorphic Adenoma (PA) is the most common tumor.
- This tumor is also known as a benign mixed tumor because histologically they are solid tubuloglandular structures alternate with myxoid and chondroid zones.
For a number of reasons, benign salivary gland tumors pose special problems for both the surgeon and their patient. First, at the outset, there is little to distinguish a benign tumor from its malignant counterpart. The diagnosis is often only made after resection and at that stage, the surgeon may wish that a more extensive procedure had been undertaken. Second, preoperative tissue diagnosis by fine needle aspiration cytology can be difficult and often inconclusive. Open biopsy at any site other than the palate is contraindicated lest seeding should develop subsequently. Third, the anatomical relationship of a tumor to the facial nerve in the parotid gland is nearly always intimate and the potential for a significant cosmetic handicap makes surgery at best challenging and certainly extremely worrying for the patient. Fourth, some patients are referred following an open biopsy, enucleation, attempted parotidectomy or with frank and extensive recurrent disease. Recurrence rates of 20-45% have been described after simple enucleation. Malignant transformation of some recurrent benign tumors is well recognized and almost impossible to cure.
There has been much evidence to suggest that radiation induces salivary gland tumors. This was initially established in epidemiological studies of those who survived the atomic bombs dropped in Japan during the Second World War.
In recent years, extreme public concern has focussed on the use of mobile telephones and the development of regional malignancies. It has been suggested that there is a relatively increased risk for brain tumors and uveal melanoma but, to date, an increased risk of salivary gland tumors has not been reported.
Most parotid and submandibular gland tumors develop in an insidious fashion, growing slowly over a long period of time without causing any other symptom whatsoever. A very small number cause discomfort by obstructing salivary flow. Pain is extremely uncommon and, if present, usually heralds malignant change. Likewise, facial weakness or palsy is virtually never seen unless the malignant change has supervened. The growth of these tumors is so slow that patients often wait many months or years before seeking attention.
Case Report
A 25-year-old lady who is a housewife, presented with left-sided neck swelling below the jaw bone for since 6 months which was progressively increasing in size without pain or skin changes. No history of fever chronic cough or other swellings in head and neck region. In past history, she gives a history of a surgery for salivary gland tumor in the submandibular region, 4 years back. Reported as Pleomorphic Adenoma of the submandibular salivary gland. Not a k/c/o any chronic disease. On examination, there was a 4x5cm firm ropy nodular non-tender swelling in the left submandibular region over the scar. No skin changes, tenderness or the local rise of temperature. Rest of the neck examination was normal. No cervical lymphadenopathy.

Salivary gland neoplasms

benign mixed tumor
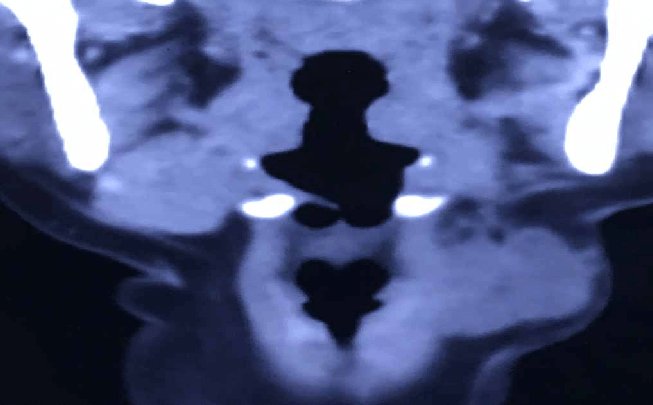
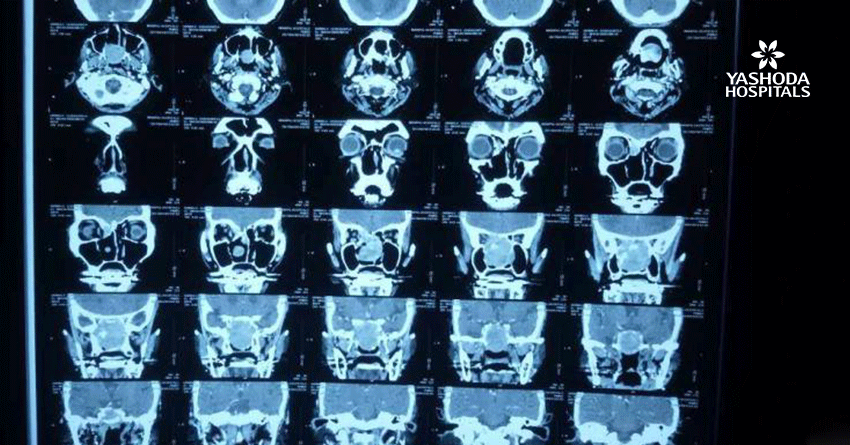
CT scan shows a mass lesion in the left submandibular region extending to the subcutaneous plane. FNAC of the lesion was done which came as Pleomorphic adenoma.
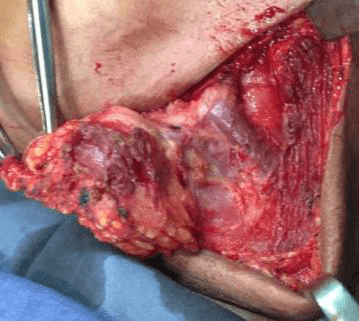
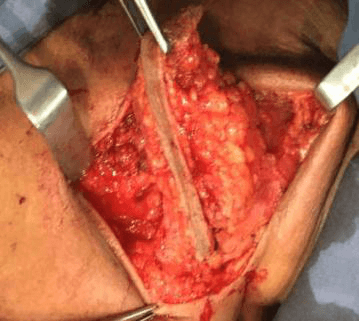
She underwent excision of the mass under GA in June 2016. The mass dissected out including the scar. The sample was sent for histopathology examination.
throat cancer hospitals in hyderabad
Jugulodigastric lymph nodes were dissected and sent for HPE. She was started on antibiotics.

Salivary gland tumors
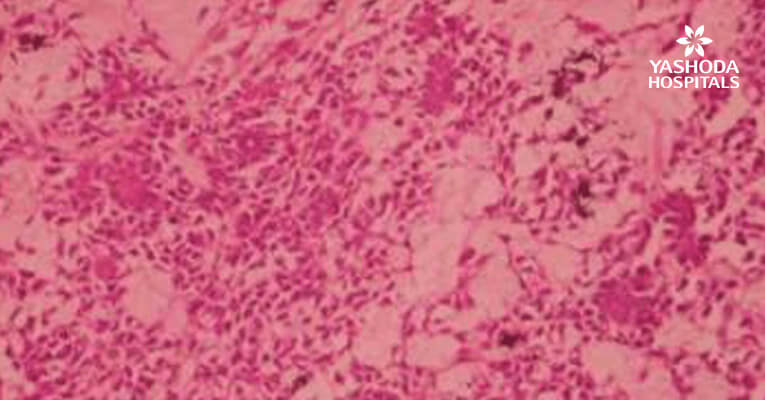
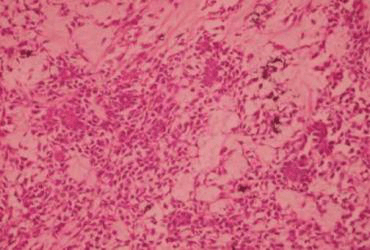
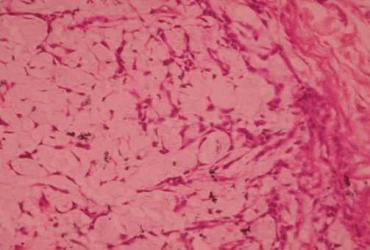
The histopathology reported as multiple circumscribed nodular lesions in the soft tissue. These are compared of myxoid looking stroma with scattered polygonal cells in intersecting cords and trabeculae. The cells have round to ovoid bland nuclei. Mitosis, nuclear atypia is not seen. Vascular tumor emboli are not seen. The impression was scar site recurrence of Pleomorphic Adenoma.
common tumor of the salivary gland
Pleomorphic Adenoma (PA) is the most common tumor
famous cancer hospital in india
top cancer hospital in india
She was comfortable post-operatively and is under follow up.
Discussion
Tumors arising in the submandibular gland present as swellings in the submandibular triangle which can be localized more accurately by bimanual palpation of the floor of the mouth. It is sometimes difficult to differentiate a tumor arising in the posterior aspect of the submandibular gland from one that is in the tail of the parotid gland. An ultrasound scan is a simple and quick method of making this distinction when doubt persists.

master health checkup in hyderabad
Recurrent tumors are often multiple and it is very easy to underestimate the precise extent of this disease. Often the tissues in the area are scarred and difficult to palpate accurately and pinpoint small foci of tumor. After all, a number of recurrences arise as a result of previous peroperative rupture of the tumor and seedlings may have been spread over a wide area.
Fine needle aspiration biopsy can be done to diagnose the tumor as in the most salivary gland tumors11. Excisional biopsy is not recommended due to the seeding potential of the tumor. We perform FNAB to diagnose the mass.
Local recurrence of the pleomorphic adenoma is related with enucleation of the primary tumor. This type of surgery is prone to recurrence due to the pseudopods of the pleomorphic adenoma. Several theories are based on the pathogenesis of the recurrent Pleomorphic Adenoma such as previous radiation of the tumor or surgical intervention which causes seeding and penetration to bloodstream or lymphatics as a reason of distant metastasis. We believe that the pseudopods of the tumors and seeding of the primary tumor are the potential reason for the pathology.
The term “Pleomorphic” refers to both histogenesis and histology of the tumor.12 The tumor has 3 components: an epithelial cell component; a myoepithelial cell component; and a stromal (mesenchymal) component. The identification of these 3 components, which may vary quantitatively from one tumor to another, is essential to the recognition of pleomorphic adenoma. Fine-needle aspiration biopsy can be done for diagnosis of Pleomorphic Adenoma.13 Histologically pleomorphic adenoma presents with the variable pattern of epithelium in a loosely fibrous stroma, which may be myxoid, chondroid, or mucoid. The epithelium is usually arranged in sheets or strands and ductal structure, often bilayered, are atypical. The myoepithelial cells are often polygonal with a pale eosinophilic cytoplasm.
The myxoid stroma of Pleomorphic Adenomas is one of its most characteristic features. It can form the major part of the tumor and can bulge into the normal gland parenchyma without any capsule intervening.
According to the World Health Organization, the characteristic of this tumor is benign in histologically but distant or local metastasis are possible.14 The almost mucoid nature of many pleomorphic adenomas makes them extremely fragile so that they can burst very easily at operation, even with the most delicate handling, unless protected by an envelope of normal glandular tissue. Rupture of the tumor inevitably seeds the operative field and can result in later recurrence.
Several points about the recurrence of these tumors are of great practical importance. First, it may take more than a decade for them to become apparent; perhaps as much as
20 years may elapse after the primary surgery before diagnosis. Claims of cures based on disease-free periods of up to ten years may, therefore, be misleading. Second, recurrences are typically multiple, frequently in the incision scar and often widely separated from each other. Finally, the incidence of malignant change is greater in recurrent tumors .15,16,17
The treatment of Pleomorphic Adenoma whether primary or recurrent is essentially surgical excision11,18-20. The excision of submandibular Pleomorphic Adenoma is usually straight forward with little or no complications due to direct surgical access. But sometimes this excision is not sufficient. Unlike the parotid where only a part of the gland is removed, total resection of the submandibular gland is always indicated for tumors.
Therefore, we conclude that when multiple masses are seen in the submandibular gland or in the region of the submandibular gland, recurrent Pleomorphic Adenoma is likely. The diagnostician should be aware of this characteristic appearance and raise the possibility of recurrent pleomorphic adenoma. We emphasize the importance of total submandibular gland excision on submandibular Pleomorphic Adenomas and superficial parotidectomy on parotid Pleomorphic Adenomas to avoid recurrence and metastasis.
References:
- EvesonJW, Cawson Salivary gland tumors: A review of 2410 cases with particular reference to histological types,age and sex distribution. J Pathol. 1985;146:51–8.
- Spiro RH Salivary neoplasms: overview of a 35 year experiencewith 2,807 Head Neck Surg.1986;8:177- 184.
- Rawson AJ, Howard JM, Royster Tumors of the salivary glands. A clinicopathological study of 160 cases. Cancer1950; 3: 445-8.
- McFarland Three hundred mixed tumors of the salivary glands of which 69 recurred. Surgery, Gynecology and Obstetrics 1936; 88: 457-68.
- Stein I, Geschickter Tumors of the parotid gland. Archivesof Surgery 1934; 28: 482-526.
- KrollsSO, Boyers Mixed tumors of salivary glands: long-term follow-up. Cancer 1972; 30: 276-81.
- BenedictEG, Meigs Tumors of the parotid gland. A study of 225 cases with complete end-results in 80 cases. Surgery, Gynecology and Obstetrics 1930; 51: 626-47.
- Wood Mixed tumors of the salivary glands. Annals of Surgery 1904; 39: 57
- Kundi M, Mild K, Hardell L, Mattsson MO. Mobile telephones and cancer – a review of epidemiological Journal of Toxicology and Environmental Health. Part B, Critical Reviews. 2004; 7: 351-84.
- Hardell L, Hallquist A, Hansson Mild K, Carlberg M, GertzenH, Schildt EB et No association between the use of cellular or cordless telephones and salivary gland tumours. Occupational and Environmental Medicine. 2004; 61: 675-9 .
- Giurana RJ, Rodado C, Saez M, Bassas C (2000) Giant parotidpleomorphic adenoma involving the parapharyngeal space: report of a J Oral Maxillofac Surg 58: 1184-7.
- Kondo A case of lipomatous pleomorphic adenoma in the parotid gland: a case report. Diagnostic Pathology 2009; 4: 16-18.
- Rodriguez KH, Vargas S, Caroline R, Perez-Atayde A, ShambergerR, McGill TJ, et Pleomorphic adenoma of the parotid gland in children. Int J Ped Otorhinolaryngeology 2007; 71: 1717-23.
- Nouraei SAR, Ferguson MS, Clarke PM, Sandison A, SandhuGS, et (2006) Metastasizing pleomorphic salivary adenoma. Arch Otolaryngol Head Neck Surg 132: 788–93.
- PiekarskiJ, Nejc D, Szymczak W, Wronski K, Jeziorski Results of extracapsular dissection of pleomorphic adenoma of parotid gland. Journal of Oral and Maxillofacial Surgery. 2004; 62: 1198-202.
- Stennert E, Wittekindt C, Klussmann JP, Arnold G. Guntinas-Lichius. Recurrent pleomorphic adenoma ofthe parotid gland: a prospective histopathological and immunohistochemical Laryngoscope. 2004; 114: 158- 63.
- MaxwellEL, Hall FT, Freeman Recurrent pleomorphic adenoma of the parotid gland. Journal of Otolaryngology. 2004; 33: 181-4.
- Batsakis JG, Sneige N (1989) Pathology consultation: parapharyngeal and retropharyngeal space diseases. Ann OtolRhinol Laryngol 98: 320-1.
- Hugues KV III, Olsen KD, MacCafferey TV (1995) Parapharyngealspace Head Neck 17: 124-30.
- Varghese BT, Sebastian P, Abraham EK, Mathews A (2003)Pleomorphic adenoma of minor salivary gland in the parapharyngeal World J Surg Oncol 1: 2.
About Author –
Dr. Nagendra Mahendra, Consultant ENT Surgeon, Yashoda Hospital, Hyderabad.
DLO, DNB (ENT)
His expertise includes micro ear surgery, phono surgery / M, endoscopic surgery, endoscopic skull base surgery & cosmetic surgery, Head & Neck related surgeries including skull base surgery & laryngotracheal surgery.


 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

