Fungal Intracranial Abscess – The bugbear in renal transplant

There can’t be anything more challenging than treating a solid organ transplant recipient with fungal infection. Many a times it is ironically said that nephrologists are so obsessed in saving the allograft kidney that they end up killing the patient. Here we present one such challenging instance of a posttransplant infection in a renal transplant recipient.
Case Report:
Mr. LP, a 62 year gentleman, with type II DM (with neuropathy and retinopathy), hypertension, hypothyroidism, chronic pancreatitis, glaucoma and end stage renal disease on hemodialysis for the past 3 years was taken up for deceased donor renal transplantation on 11-09-2015. The deceased donor happened to be an expanded criteria donor. The donor was 52 years old, had hypertension for about 6 years and had suffered a hemorrhagic stroke. Induction was given with two doses of basiliximab along with methylprednisolone (MP) 500 mg once a day on the day of transplant and post-operative day (POD) 1 and 250 mg on POD2. He was also started on tacrolimus (0.07 mg/day) and MMF (2 gm/day) from the time of transplant. From POD3 prednisolone, 20 mg/day, was substituted for MP. He was also started on valgancyclovir, cotrimoxazole and fluconazole at the same time. The patient was discharged from the hospital on the 8th POD with a serum creatinine of 2.3 mg/dl and a good urine output. At the end of one month following the transplant his serum creatinine had improved to 1.6 mg/dl, hence the dose of prednisolone and MMF were reduced by 50%. He was followed up once a fortnight.
On 12-11-2015 he was presented with fever, malaise and ataxia which he was experiencing from the previous day. Evaluation revealed he a deep seated abscess in the right hemisphere of the cerebellum, multiple areas of consolidation in both the lungs and abscesses over the chest and abdominal wall. Pus aspirated from the chest wall and Broncho alveolar lavage revealed aspergillus. A diagnosis of disseminated aspegillosis including was made. MMF was stopped, tacrolimus was reduced to maintain a trough level of 3 ng/ml and prednisolone was reduced to 5 mg once a day. He was also started on amphotericin B deoxycholate and voriconazole simultaneously. The idea of neurosurgical intervention of the cerebellar abscess was abandoned after careful deliberation with the neurosurgical team. By the end of one week, with the above interventions, his fever had subsided, malaise had improved significantly and ataxia a little bit. His serum creatinine had increased to 3.5 mg/dl. Amphotericin B deoxycholate and voriconazole were continued for another one week with a close watch on his allograft kidney function.
By the end of 2nd week of therapy a repeat MRI of the brain showed the cerebellar abscess to have reduced a little in size along with a substantial reduction of the surrounding edema. His serum creatinine had increased to 5.2 mg/dl. Biopsy of the allograft kidney was performed and it did not reveal rejection. The renal dysfunction was considered to be amphotericin B induced. Hence amphotericin B was stopped and voriconazole was continued. He remained on dual immunosuppression as mentioned above. By the third week of therapy his serum creatinine reached his previous baseline of 1.6 mg/dl. Voriconazole was stopped after 2 years.
Now three years following the transplant the patient is healthy with a serum creatinine of 1.4 mg/dl and minimal cerebellar s ign s . He r e m a i n s o n m i n i m a l do s e s o f du a l immunosuppressive drugs.
Discussion and conclusion:
Fungal brain abscesses in post-renal transplant recipients lead to a very high mortality despite neurosurgical intervention and the use of appropriate antifungal drugs. There are very few cases in literature where a successful outcome was achieved without a neurosurgical intervention. Here we present a patient who was successfully treated without neurosurgical intervention. Early diagnosis, institution of appropriate antifungal therapy coupled with an immediate reduction in immunosuppression which included a complete withdrawal of antimetabolite was instrumental in the successful outcome of this patient.
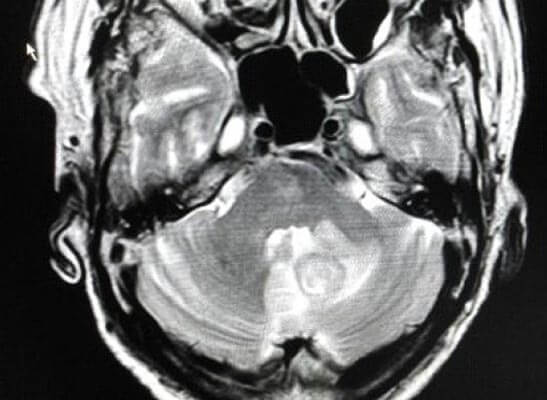
MRI brain at presentation

MRI brain 4 months later

HRCT chest at presentation
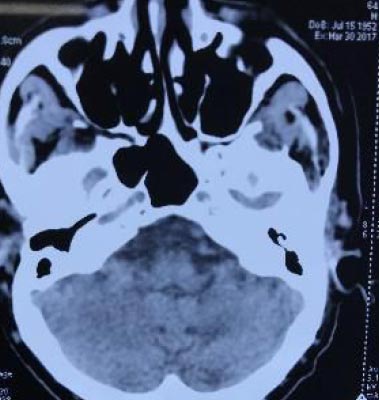
CT brain 1.5 years later
About Author –



 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

