Intraoperative MRI in endoscopic transsphenoid pituitary surgery for pituitary adenoma

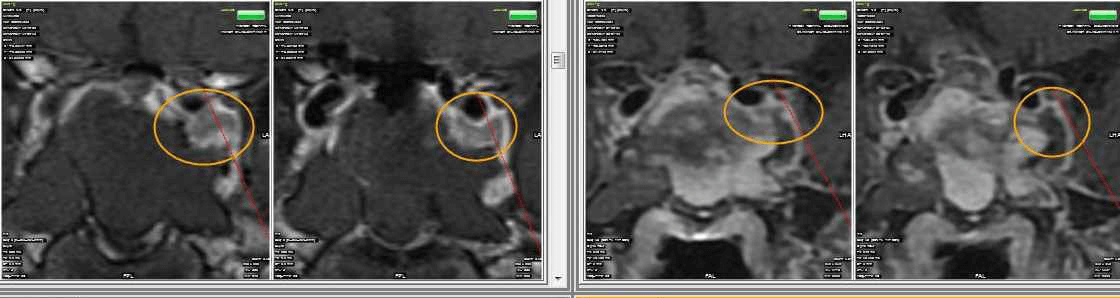
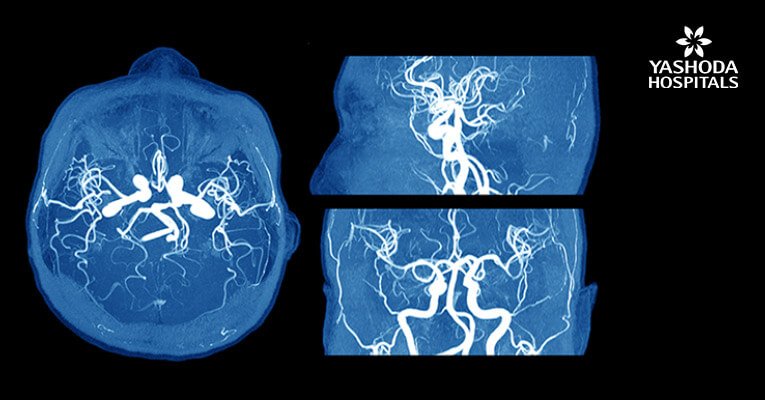
65 year old male with Pituitary Macroadenoma with cavernous sinus extension. Endoscopic Transsphenoidal Surgery done with Intraoperative MRI showing residual tumor in the cavernous sinus region under the left carotid artery. Post op MRI showing on the right no residual tumor in the sinus. (T1 contrast above and T2 coronal sections below).
Excision of pituitary tumors is achieved well in most cases. But in Macroadneomas with lateral and superior antreo- posterior extensions it is difficult to achieve total excision. This would usually necessiate Radiotherapy at later date. Radiotherapy has higher chance of Hypopituitarism too. If intra-operatively the residual tumor is seen with MRI, then total excision can be possible in almost all the cases. This would avoid unncessary radiation in these patients with benign tumors. This also increases preservation of normal functioning pituitary gland. It is invaluable in functioning adenomas where surgery has the highest chance of cure.
Case 1: 35/ M
- Pre-operative Coronal and Sagittal contrast enhanced T1W images show a well circumscribed homogenously enhancing sellar mass with suprasellar extension (Figure 1).
- Intra-operative coronal and sagittal T1W (Figure 2) contrast enhanced sequences show no residual enhancing tumour in the post operative bed (Figure 3).
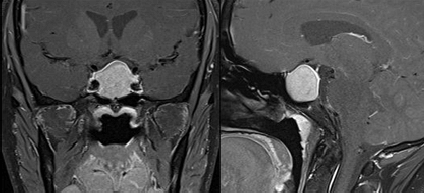
Figure 1
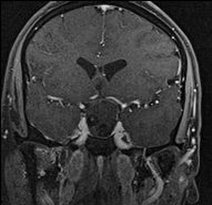
Figure 2
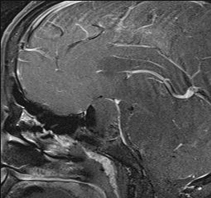
Figure 3
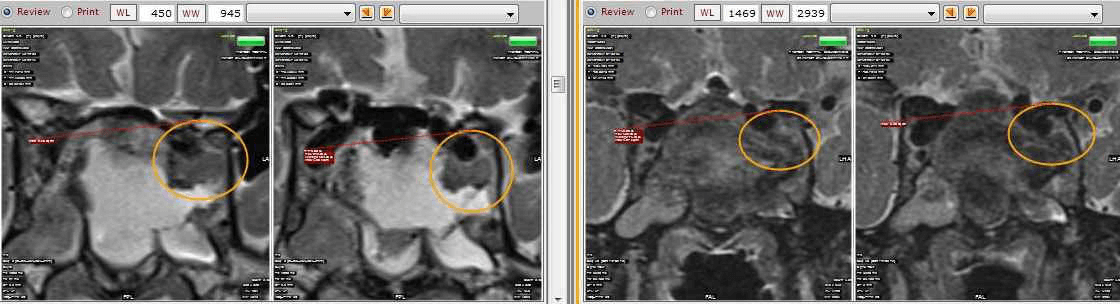
Case 2: 35/ M
- Pre-operative sagittal contrast enhanced T1W image shows a sellar mass with suprasellar extension (Figure 4)
- Intra-operative MRI (Figure 5) shows residual enhancing tumour, which was then taken up again for resection. Post operative MRI (Figure 6) shows a thin enhancing capsule with no residual tumour.
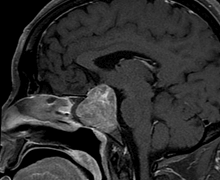
Figure 4
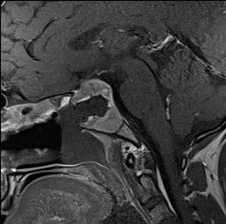
Figure 5
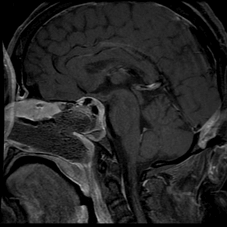
Figure 6
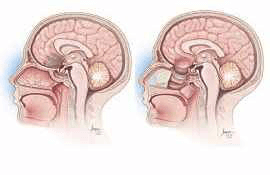
Pituitary tumors are common benign tumors which have been treated with surgical excision followed by radiotherapy for residual disease. The surgery for these tumors have been popularly done mainly by transcranial approaches. Though transnasal approach was tried initially by pioneers in neurosurgery, it was not popular due to lack of good illumination and guidance. With advent of endoscopic techniques and Endoscopic Neurosurgery as such, Transnasal Transsphenoidal Surgery has become standard now for pituitary tumors. Moreover with Neuronavigation and intra-operative imaging with Intraoperative MRI, total excisions are more often possible and post-operative radiation avoided completely for these benign lesions. The preservation of normal Pituitary with its function too has gone up with endoscopic resections, intra-operative imaging and avoidance of radiation.
Endoscopic Transsphenoidal Pituitary Surgery is a new frontier in endoscopic transnasal procedures in ENT and Neurosurgery. It is a four hand technique involving the Neurosurgeon and ENT surgeon, where both work together through both nasal cavities simultaneously.
The role of the ENT surgeon primarily lies in two stages. First in creating an adequate operating access through the nose for the Neurosurgeon and exposing the pituitary tumour which lies in the sella, by creating a wide sphenoidotomy, removing the posterior nasal septum, and if required, posterior ethmoid cells (for tumours which extend laterally into the cavernous sinus).
After removal of the tumour, reconstruction of the sella defect and effectively closing a CSF leak if encountered, are the closing steps of the surgery. The role of the Nasoseptal Flap comes into play at this stage.
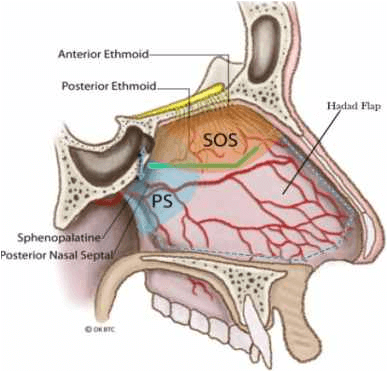
The vascularised Nasoseptal Flap (based on the septal branch of the Sphenopalatine Artery) deserves a special mention; also known as the ‘Hadad’ flap, it is the workhorse in sella and sphenoid defect reconstructions after Transsphenoid Surgeries. It is harvested at the beginning of the procedure and kept in the nasopharynx to be used at the end of the surgery.
We also use a lumbar drain to drain CSF during the procedure which reduces the arachnoid bulge in to the operative field. This minimises the chance of CSF leak. If a CSF leak does occur, we keep the drainage of CSF going for 3 to 5 days to facilitate healing of the repair of the sellar floor done with the mucoperiosteal flap.
The Hadad flap comes with its own set of problems for the patient, in the form of long term crusting and nasal obstruction (due to exposed septal cartilage and bone). To overcome these problems, We at Yashoda Hospitals, Secunderabad, use a modified version of the Hadad Flap, called the ‘Rescue Flap’, which is an incomplete elevation of the Nasoseptal Flap without compromising the sphenoid and sella exposure. This rescue flap can be converted into a Hadad if need be, or the septal flaps can be replaced back on to the nasal septum. This has reduced post-operative nasal crusting, improved healing time and reduced review visits to the ENT OPD.
About Author –
Dr. Anandh Balasubramaniam, Senior consultant and HOD, Neurosurgery, Yashoda Hospital, is a renowned neurosurgeon in Hyderabad. His expertise include neuro-oncology, intraoperative MRI and image guided neurosurgeries, endoscopic surgeries, endoscopic minimally invasive surgeries, deep brain stimulation and functional neurosurgeries.






 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More