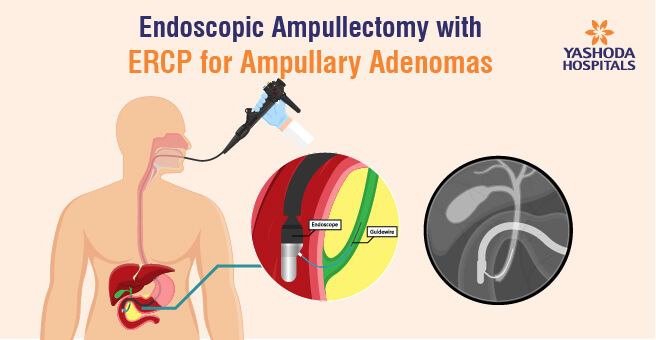
Endoscopic Ampullectomy with ERCP for Ampullary Adenomas
Introduction
Ampullary adenomas are growths found near the vater, a small opening where the common bile duct and pancreatic duct join and empty into the small intestine. These lesions, often discovered incidentally during endoscopy or investigations for unexplained bile duct and pancreatic dilation, are slow-growing lesions. They are also associated with familial adenomatous polyposis syndromes. Over time, they can progress from being benign to pre-malignant and, if undetected, may develop into ampullary carcinomas. Depending on the stage of diagnosis, these adenomas can exhibit various presentations, ranging from low-grade dysplasia to high-grade dysplasia, early malignancy, or invasive carcinoma.
Historical Management and Evolving Approach
Traditionally, radical resection, such as Whipple’s procedure, was the standard treatment for ampullary adenomas, but it carried significant morbidity and mortality risks. Subsequent limited surgical resection improved these risks but still led to high recurrence rates, especially in cases of high-grade dysplastic lesions. However, the current approach emphasizes successful endoscopic resection using EMR (Endoscopic Mucosal Resection) techniques, particularly for small (1-2 cm) malignant lesions. This procedure, followed by biliary and pancreatic ductal stenting, helps minimize the risk of post-procedure pancreatitis. Endoscopic procedures show reduced morbidity and almost no mortality, although there’s a slight increase in risks like pancreatitis and local bleeding. Remarkably, in pre-malignant, low-grade dysplastic polyps, Endoscopic Ampullectomy serves as a curative method with minimal recurrence rates.
Advantages of Endoscopic Ampullectomy
Endoscopic Ampullectomy emerges as an excellent option, particularly for elderly patients with comorbidities, who may not tolerate radical resections. This procedure provides a way to manage ampullary adenomas with reduced morbidity. Regular follow-ups at six-month intervals are recommended to monitor any signs of recurrence. Even in cases of advanced pre-malignancy with significant high-grade dysplasia localised to the ampulla, Endoscopic Ampullectomy has a favourable prognosis, with a recurrence rate of approximately 20% upon follow-up. Overall, this minimally invasive procedure, performed under sedation, allows for a 24-hour discharge, offering a promising therapeutic approach to managing ampullary adenomas.
About Author –
Dr. Santosh Enaganti, Senior Consultant Gastroenterologist & Hepatologist, Advanced Interventional Endoscopist , Yashoda Hospitals – Hyderabad
MD, MRCP, CCT (Gastro) (UK), FRCP (London)





 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

