Cesarean sections in cath lab – Uterine artery embolization. Life-saving for the mother!

OUR MOTTO:
” Save the Mother – Save the Child – Save the Uterus”
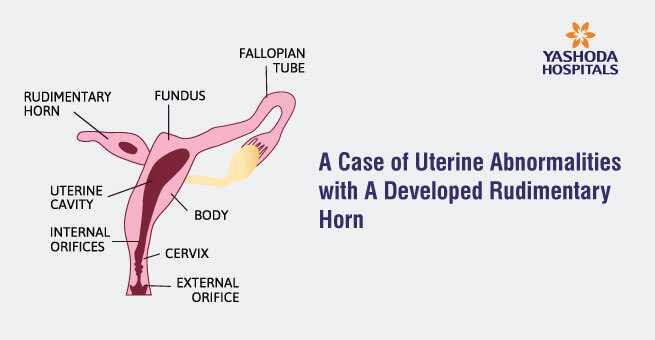
The biggest nightmare for any obstetrician or gynecologist would be postpartum hemorrhage on the table. Particularly, if it is due to abnormal placentation like central placenta previa (accreta or increta).
Another deadly combination in pregnancy would be multiple fibroids, which totally alter the anatomy of the uterus. In these conditions, the regular compression sutures or tamponade may not give ideal results.
The blood flow in the uterine artery rises from a mean of 94.5ml/ min before pregnancy to a mean of 342 ml/ min in late pregnancy, reflecting a 3 to 5 fold increase in each uterine artery. The mean diameter of the vessel increases from 1.6 mm to 3.7 mm towards term. Due to these gross hemodynamic changes, it is sufficient to exsanguinate a pregnant woman during the Lower Segment Cesarean Section (LSCS) within 10 minutes.
These changes were kept in mind. With a vision to reduce the amount of transfusion of blood and blood products, a hybrid treatment was planned for a few of our patients. It would help to save the uterus and to decrease the morbidity and mortality associated with torrential blood loss, thereby avoiding subsequent multiple transfusions. The hybrid treatment adopted involved, uterine artery embolization during C-section, which resulted in excellent results in terms of saving the uterus, decreasing blood loss, and decreasing the need for multiple blood transfusions.
Patient I
Mrs. X, G3P1L1A, presented to us at 30 weeks of gestation with multiple episodes of per vaginal (PV) bleeding. On investigation, including an MRI scan, she was diagnosed with major placenta previa with focal accreta. She was hospitalized at 34 weeks and given betresol cover. At the end of 35 weeks, in view of PV bleeding, she was subjected to elective ISCS with uterine artery embolization. The patient delivered a live baby of 2.4 kgs followed by embolization, then placental removal was done. The patient had 1.5 liters of blood loss, and it was corrected with 2 units of PRBC, 2 units of PRBC, and 2 units of FFPs. She was discharged in hemodynamically stable condition on day 3 after surgery without any complications. The patient continues to have regular periods without any long term sequelae.
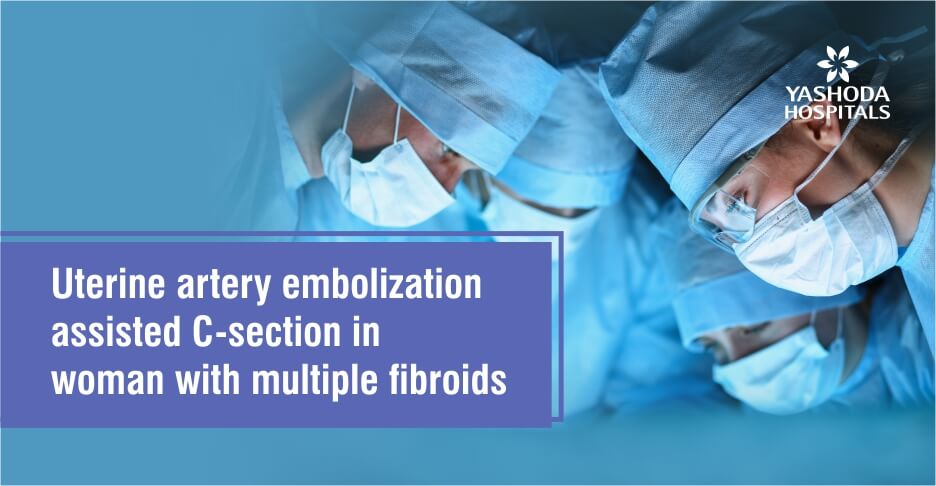
Patient II
Mrs. X, aged 29 years, with a previous history of myomectomy for multiple fibroids 2 years ago, presented to us with early pregnancy. On examination, the patient was found to have multiple fibroids that were complicating early pregnancy. After counseling, the patient and the family continued pregnancy until 36 weeks with nil complaints and complications. At 36 weeks, she had multiple fibroids with a breech presentation. A decision was made to deliver the baby by Lower Segment Cesarean Section (LSCS) and Uterine Artery Embolization (UAE). She delivered a live baby of 2.7kg. Before the removal of the placenta, UAE was done using gel foam, PUA particles, and glue followed by placental removal. Though the uterus did not retract well due to multiple fibroids, she hardly had any bleeding. The lower segment was closed in 2 layers. The post-op period was uneventful, and the patient did not require any blood product transfusion.
Patient -III
A 38 years elderly primigravida, post-IVF conception, came to us for regular antenatal care and safe delivery, She was diagnosed with central placenta previa on routine ultrasound. She had PV spotting a couple of times, which was managed conservatively. At 28 weeks gestation, she presented with heavy PV bleeding which did not respond to conservative management. After betresol and Mgso4 cover, she had to be taken up for emergency LSCS in the cath lab with 3 units of PRBC. LSCS with UAE was done, and a live baby of 1.3kg was delivered as breech. Hemostasis was good, with minimal blood loss, but on ‘0’ post-op day, the patient complained of numbness of the right leg. A check angiogram was done, a thrombus was present in the right Enzyme immunoassay (EIA) for which suction thrombectomy was done. The patient recovered well, and the baby was discharged after 2 months. Both the mother and the child are doing well.
Patient -IV
A primigravida, married for 3 months, presented to us with 40 days of amenorrhea. On examination, the uterus was 16-18 weeks size with an irregular surface. On ultrasound examination, she was found to be 5-6 weeks pregnant with multiple fibroids, and the largest measured 10 cms. After a lot of discussions, she planned to continue the pregnancy and did so till term without any complications. At 37 weeks, a decision was made to have elective ISCS with UAE. So on the 13th of September 2019, the patient was subjected to ISCS with bilateral UAE. The surgery was uneventful with absolutely non-PPH. The patient went home on day 3 after the surgery. Further follow up is awaited.
At our center, Uterine Artery Embolization (UAE) is also done for patients with secondary PPH, who are diagnosed with AV malformation or pseudoaneurysm of uterine artery.
This procedure is also done in patients with scar ectopic and AV malformations following MTPS. These patients have excellent recovery without the need for major surgeries or hysterectomy.
About Author –
Dr. Bhagya Lakshmi S, Consultant Obstetrics, Gynecologist & Laparoscopic Surgeon, Yashoda Hospital, Hyderabad
MD (OBG)
Specialized in management of high-risk pregnancies and painless labor. Dr. Bhagya Lakshmi S treats fertility problems, PCOS and other gynecological conditions.





 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

