Acute onset quadriplegia as a complication of hepatitis-A infection
Background
A 14 year old boy was brought to the emergency department with history of sudden onset of neck pain, one episode of non-bilious vomiting after getting up from bed followed by weakness of lower and upper limbs which progressed to truncal and respiratory muscle weakness over few hours. He reported tight band like sensation over the upper chest and developed urinary retention. There was no history of headache, seizures or altered sensorium. No history of trauma or external bleeding manifestations. He had a history of fever with jaundice 14 days back, evaluated at a local hospital and diagnosed as viral hepatitis A; he was treated symptomatically and got discharged in a stable hemodynamical status with icterus.
Clinical Examination
On examination, patient was moderately built and nourished. Vitals were pulse rate of 104/min, blood pressure 110/70 mm of Hg in right arm, respiratory rate of 30/min, Spo2 98% in room air, temperature 99 degree F. Single breath count (SBC) was 8. General examination revealed deep icterus, cardiovascular examination and chest auscultation were unremarkable and abdomen was soft. On neurological examination he was conscious, irritable, obeying commands, pupils were bilateral 2mm reacting to light, no nystagmus, normal fundus, no facial weakness and other cranial nerves examination was grossly normal. He was unable to lift his neck against gravity. Power in all 4 limbs was grade 1/5 with hypotonia and DTRs were absent with extensor plantars. Sensory level was at T5/T6 level and he had urinary retention.
Diagnosis And Treatment
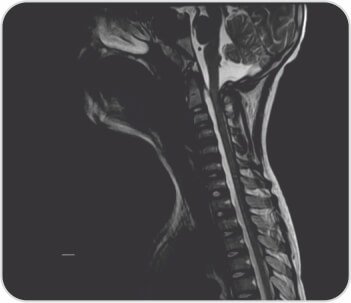
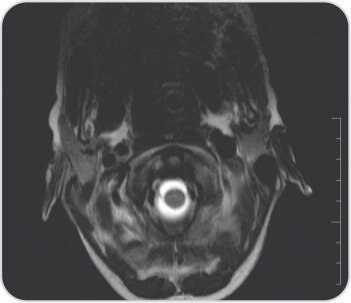
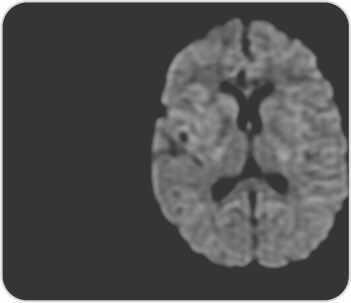
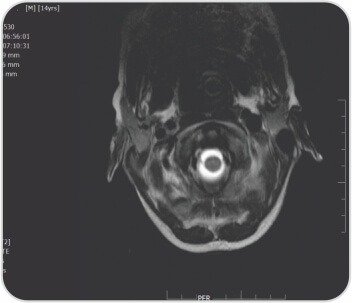
MRI of whole spine with brain revealed long segment anterior epidural collection which was hyperintense on T2 and hypointense on T1 with layering seen extending from C2 to D8 level causing posterior displacement and compression of cervical and dorsal cord- likely hemorrhage, mild sprain of posterior paraspinal soft tissues in cervical region noticed. Laboratory investigations revealed Hb7.5gr%, TLC11, 700/mm3, platelets2.92lakhs/mm3, Rbs 96 mg/dl, Serum creatinine 0.5mg%, Bl.urea 37.0 mg%, Serum Na+ 128, S.K+ 3.6, S.Cl- 93.0 meq/l. Liver function tests grossly deranged with Total Bilirubin 21.90 mg% (Direct 13.70 Indirect 8.20) SGPT 254u/l SGOT 180 u/l Alk phosphatase 265.00, Total proteins 6.00 g% (Alb 2.80,Glb 3.20 g%). PT 68.0 sec INR >8.0, APTT 86.8 sec. HAV IgM antibody positive: 2.62; HBsAg, HBeAg, HCV, HIV: Not-Reactive; ANA profile was negative. He was admitted in intensive care unit and received 7 units of FFPs, 3 PRBCs along with parenteral Vitamin K injections and ventilatory supportive care. Neuro surgery consultation followed by C3- C6 laminoplasty with evacuation of hematoma done on day 2 of admission. On day 5, tracheostomy was done and gradually weaned of ventilator. He was discharged on day 15 with bipap support to rehabilitation centre. Quadriplegia was persisting with grade 2 power in upper limbs and total Bilirubin 2.90 mg/dl, SGPT 157, SGOT 68u/l at the time of discharge. At two weeks follow-up he improved further with spastic quadriplegia – grade 2 power in all limbs, stable hemodynamics and normal liver function tests.
Conclusion
Neurological complications from hepatitis A are very rare, including encephalitis, meningoencephalitis, meningitis, Guillain-Barre syndrome, chronic inflammatory demyelinating polyradiculoneuropathy, sensory neuropathy, mononeuropathy simplex and multiplex, myasthenia gravis, myopathy, and transverse myelitis. Our patient had grossly deranged liver function tests and obvious laboratory evidence of coagulopathy at the time of onset of quadriplegia. In view of the supportive imaging evidence and positive serology for hepatitis A final diagnosis of coagulopathy induced spontaneous spinal epidural hematoma as a complication of viral hepatitis A was made.
About Author –
Dr. Kiran Kumar Varma
MBBS, MD, MEM, DEM
Consultant Emergency Physician,
Yashoda Hospitals, Malakpet







 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

