Acute Kidney Injury with Hemoptysis: A Formidable Clinical Challenge

Introduction
Granulomatosis with polyangiitis (GPA), formerly known as Wegner’s granulomatosis, is one of three ANCA-related vasculitides. An environmental trigger in genetically susceptible individuals results in the production of pathogenic antibodies, anti-neutrophil cytoplasmic antibodies (ANCAs), which leads to necrotising small and medium vessel vasculitis. Early detection and treatment are critical in preventing irreversible renal damage.
Case Report
Mr. RK, 67, a diabetic and hypertensive with a history of low-grade fever, cough with hemoptysis, breathlessness, and decreased urine output, presented with a four-day history of these symptoms.
On arrival, he was hypoxic (SPO2- 90%), his blood pressure was 150/90 mm of hg, his temperature was 99.5 f, and he had pedal edoema. His serum creatinine level was 3.6 mg/dl, his urine showed 3+ albumin with 20 to 25 RBCs/HPF, and his chest radiograph revealed nodular opacities. His coagulation profile was normal, and there was no evidence of infection. The possibility of pulmonary-renal syndrome, most likely GPA, was considered.
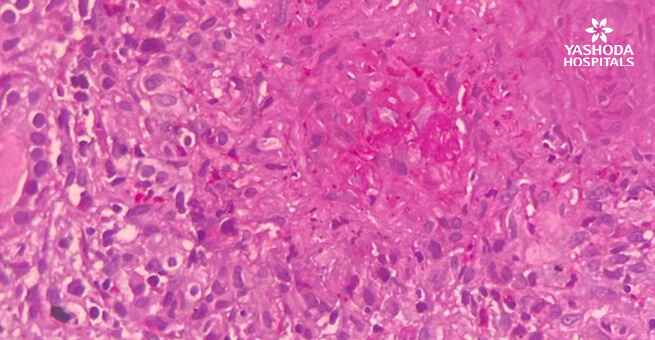
He was immediately taken up for hemodialysis because he was oliguric and had severe metabolic acidosis in ABG. After three sessions of hemodialysis, a renal biopsy was performed, which revealed necrotizing granulomatosis crescentic glomerulonephritis (Fig 1 and 2), which was pauci immune on immunofluorescence studies (Fig 3). PR3-ANCA was found to be positive. This confirmed the GPA diagnosis. He was also given plasmapheresis five times because he had significant hemoptysis.
Along with other supportive measures, he was started on methylprednisolone and cyclophosphamide. Over the next three weeks, his renal function improved, and hemodialysis was discontinued.
He now has a stable renal function, with a serum creatinine of 1.9 mg/dl, 14 months after his diagnosis, and is asymptomatic. As for maintenance therapy, he is now receiving prednisone along with Rituximab.
Discussion
In the elderly with a history of recurrent sinusitis and/or pneumonia episodes, GPA manifests as a pulmonary-renal syndrome. ANCAs are pathogenic antibodies. In vitro studies show that cytoplasmic ANCAs are translocated to the cell surface once neutrophils are primed by cytokines in a genetically susceptible individual. Neutrophils that have ANCAs on their cell surfaces bind to the antigens and become activated. These activated neutrophils infiltrate the small and medium vessel walls, causing necrotising vasculitis in the kidneys and lungs.
A renal biopsy is essential for diagnosis, management, and prognosis, and it should be performed as soon as possible. Immunosuppressive medications such as corticosteroids, cyclophosphamide, rituximab, azathioprine, and mycophenolate are commonly used in treatment. Cyclophosphamide plus plasmapheresis is preferred over rituximab during remission induction in patients with severe disease or hemoptysis. Plasmapheresis is required in patients who also have anti-GBM antibody disease.
Conclusion:
GPA is an aggressive disease that affects the elderly and must be diagnosed early for proper management. Due to the early diagnosis by renal biopsy, timely administration of methylprednisolone along with cyclophosphamide, performing plasmapheresis during the induction phase, and continuing therapy with prednisone next and rituximab in the maintenance phase, our patient was able to be treated with excellent results.
Figure 1: Core showing 3 glomeruli

Figure 2: High power view of the glomeruli with circumferential crescent with peripheral giant cell reaction.

Figure 3: No immune deposits on immunofluorescence.

About Author –
Dr. Sashi Kiran A, Consultant Nephrologist, Yashoda Hospitals – Hyderabad
MD (Pediatrics), DM (Nephrology)



 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

