A Curious Case of Hemoptysis – Thinking Out of the Box
Introduction:
A 35-year-old female nurse, having recently completed treatment for multidrug-resistant (MDR) cervical node tuberculosis with an all-oral bedaquiline-based regimen, presented with a perplexing six-month history of streaky hemoptysis. Despite lacking other constitutional symptoms, her persistent cough and hemoptysis raised concerns, prompting further investigation.
Diagnostic Evaluation:
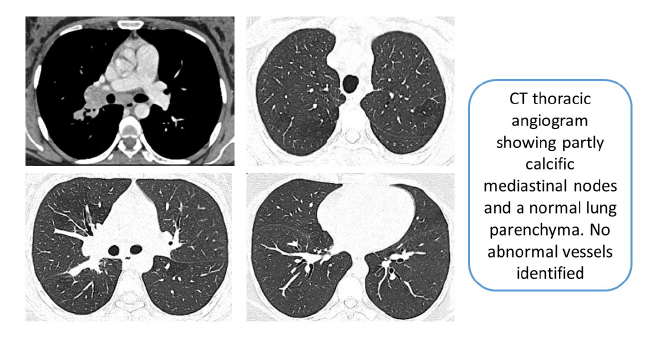
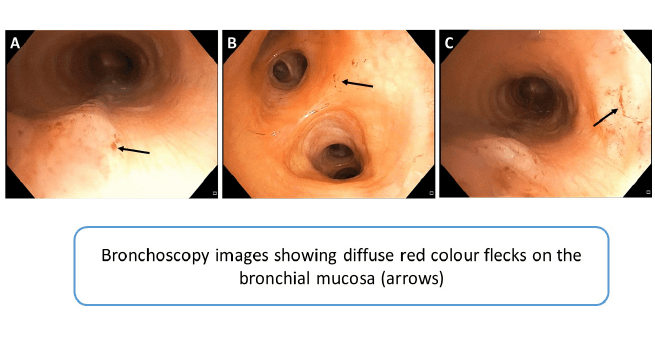
A CT thoracic angiography did not reveal abnormal vessels, while lung parenchyma appeared normal, albeit with a few mediastinal nodes. A previous bronchoscopy reported normal findings. However, upon presentation to our center, repeat bronchoscopy uncovered red flecks throughout the bronchial tree, raising suspicion.
Microbiological Workup:
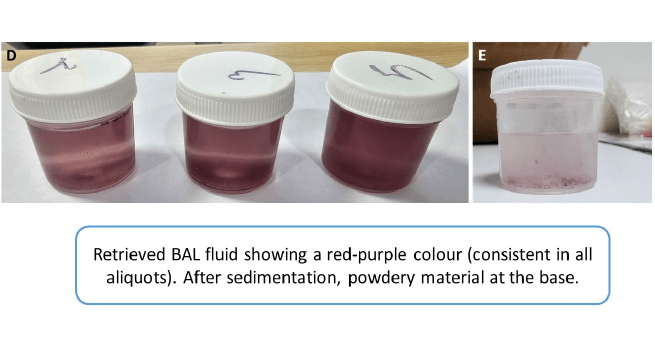
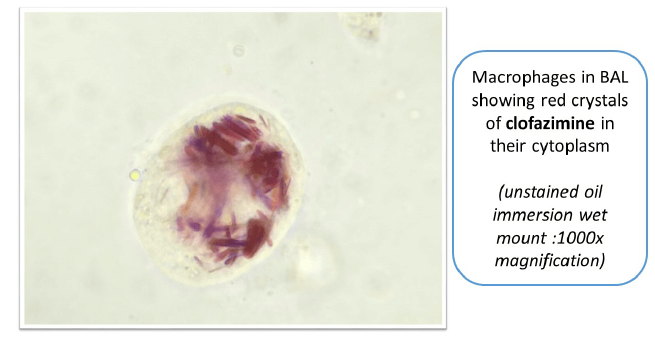
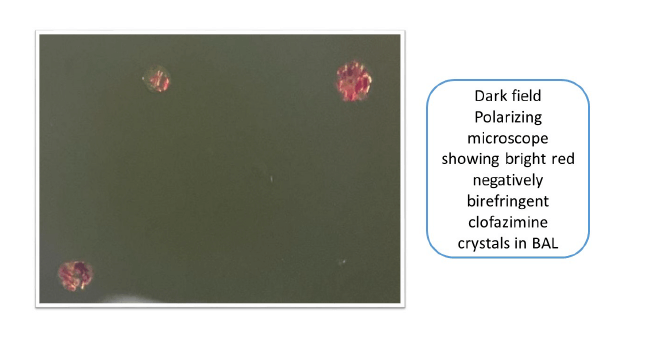
Bronchoalveolar lavage (BAL) exhibited a reddish-purple return, with centrifugation revealing a powdery purple substance. Microbiological analysis showed positive Xpert MTB, consistent with healed tuberculosis. However, no active infection was detected.
Investigative Insights:
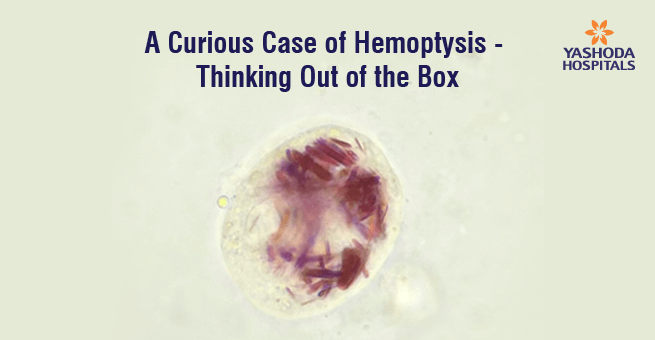
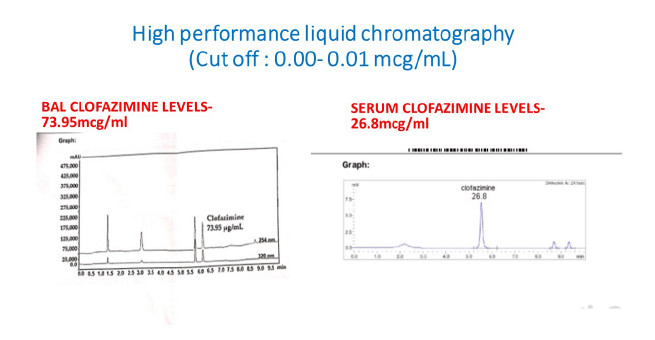
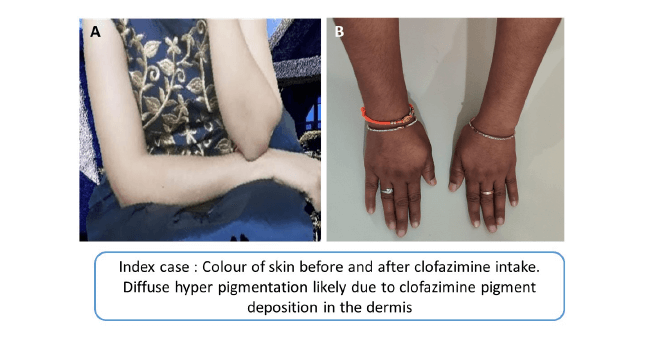
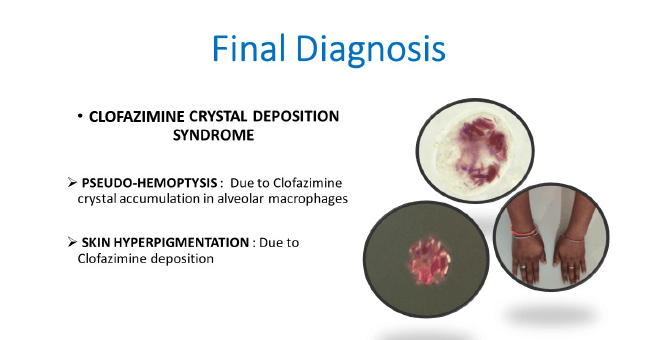
Given the unusual findings, further investigation into clofazimine deposition was undertaken. Serum and BAL clofazimine levels were analyzed using high-performance liquid chromatography (HPLC), revealing markedly elevated BAL levels. Microscopic examination of BAL fluid revealed alveolar macrophages filled with reddish crystals of clofazimine. Additionally, the patient exhibited diffuse hyperpigmentation of the skin.
Diagnosis:
Based on the investigative findings, a diagnosis of Systemic Clofazimine Crystal Deposition Disorder was confirmed. This rare syndrome is presented as pseudo-hemoptysis, with clofazimine crystals deposited systemically causing respiratory symptoms.
Final Diagnosis:
Clofazimine Crystal Deposition Syndrome leading to Pseudo-Hemoptysis.
Conclusion:
This case underscores the importance of thorough investigation and critical thinking in diagnosing atypical presentations of medical conditions. Systemic clofazimine crystal deposition disorder, though rare, should be considered in patients with a history of clofazimine use presenting with respiratory symptoms mimicking hemoptysis. Early recognition and diagnosis can prevent unnecessary interventions and guide appropriate management strategies.






 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

