Understanding PCL Injuries: What You Need to Know
Overview of PCL injuries
Introduction
The Posterior Cruciate Ligament Injury (PCL) is one of the key ligaments located in the knee, playing a crucial role in maintaining knee stability. While less common than Anterior Cruciate Ligament (ACL) injuries, PCL injuries can be equally debilitating. Understanding the nature, causes, symptoms, and management of PCL injuries can help individuals take proactive steps toward recovery and prevention.
What is a PCL Injury?
The PCL is a strong band of tissue that connects the thigh bone (femur) to the shinbone (tibia) at the back of the knee. It works in conjunction with the ACL to control the back-and-forth motion of the knee. A PCL injury typically occurs when there is a direct blow to the front of the knee while it is bent, such as in car accidents or sports-related incidents.
How do PCL Injuries occur?
PCL injuries often result from high-impact events. Hyperextended knees are one of the most common causes of PCL injuries. Some of the common causes include:
- Automobile Accidents: A direct impact to the knee during a collision.
- Sports Injuries: Contact sports like football, soccer, and basketball, where sudden stops, twists, or impacts are frequent.
- Falls: Landing hard on a bent knee can overstress the PCL.
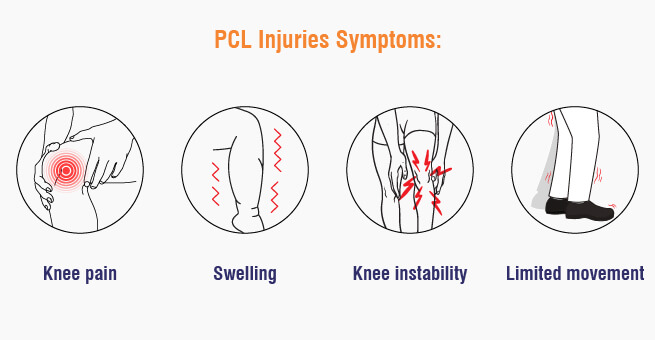
Symptoms of PCL Injuries
Recognizing the PCL injury symptoms is crucial for timely intervention. Key PCL tear symptoms include:
- Knee Pain: Pain at the back of the knee, which can be immediate or develop gradually.
- Swelling: Swelling within hours of the injury.
- Instability: A feeling that the knee is “giving way” or unstable.
- Limited Movement: Difficulty in moving the knee or bearing weight on it.
Don’t Ignore Knee Pain After A Fall; Get A PCL Injury Diagnosis Today!
Diagnosis And Treatment For PCL Injuries
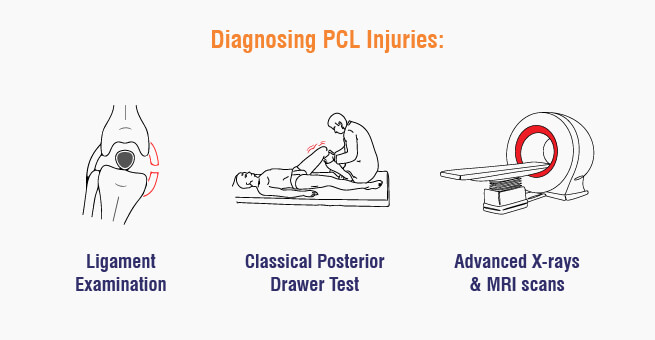
Diagnosing PCL Injuries
Diagnosis of a PCL injury typically involves:
- Physical Examination: A healthcare professional will check for tenderness, swelling, and instability in the knee.
- Classical Posterior Drawer Test: Posterior Trampletion of Tibia.
- Imaging Tests: X-rays may be used to rule out bone fractures, while advanced MRI scans provide detailed images of the ligament damage.
Management and Treatment
The posterior cruciate ligament injury treatment varies based on the severity of the injury and the patient’s activity level.
- Non-Surgical Treatments
For minor PCL injuries, non-surgical methods are often effective:
- RICE Protocol: Rest, Ice, Compression, and Elevation help reduce swelling and pain.
- Physical Therapy: Strengthening and flexibility exercises to restore knee function and stability.
- Bracing: A specialized knee brace with knee extension can provide additional support and prevent further injury.
Surgical Treatments
Severe PCL injuries or those not responding to conservative treatments may require surgery:
PCL Reconstruction: This involves using a graft (often taken from another tendon in the patient’s body) to replace the damaged ligament.
There are two primary methods for treating PCL tears: open surgical methods and arthroscopic methods.
1) Open Surgical Methods
Open surgical methods involve making a larger incision to directly access the knee joint. This approach allows the surgeon to have a clear and direct view of the structures within the knee.
Advantages:
- Provides a more direct view and access to the injury.
- Allows for the possibility of more complex reconstructions and repairs.
Disadvantages:
- Larger incision leading to more postoperative pain.
- Longer recovery time and increased risk of complications such as infection.
Indications:
- Severe multi-ligament injuries.
- Cases where arthroscopic methods may not provide adequate access or visualization.
2) Arthroscopic Methods
Arthroscopic surgery involves using a small camera (arthroscope) inserted into the knee joint through small incisions. This minimally invasive technique allows for the visualization and treatment of the PCL tear without the need for a large incision.
Advantages:
- Smaller incisions, leading to less postoperative pain.
- Reduced risk of infection and faster recovery times.
- Enhanced cosmetic outcomes due to smaller scars.
Disadvantages:
- May not be suitable for very complex or severe injuries.
- Requires specialized surgical skills and equipment.
Indications:
- Isolated PCL tears.
- Patients seeking quicker recovery and less postoperative pain.
Surgical Procedure Comparison
- Graft Choice:
- Both methods can use autografts (patient’s own tissue) or allografts (donor tissue).
- Common autografts include the hamstring tendon or the patellar tendon.
- Surgical Techniques:
- In open PCL surgery, the torn ligament is often reconstructed using a graft, and fixation devices like screws are used to secure the graft in place.
- Arthroscopic surgery typically involves the same reconstruction techniques but is performed using specialized arthroscopic instruments.
- Postoperative Care:
- Both methods require postoperative rehabilitation, which includes physical therapy to restore range of motion, strength, and stability.
- Weight-bearing and activity restrictions may vary depending on the extent of the PCL surgery and individual patient factors.
- Outcomes:
- Success rates are generally high for both methods, but individual outcomes can vary based on the severity of the tear, surgical technique, and adherence to rehabilitation protocols.
Recovery and Rehabilitation from PCL tears
PCL injury recovery times vary greatly from person to person. However, recovery from a PCL injury can take several months. A structured rehabilitation program is critical for a successful recovery:
- Initial Phase: Focus on reducing pain and swelling.
- Intermediate Phase: Gradual introduction of strength and flexibility exercises.
- Advanced Phase: Return to sport-specific training and activities.
Preventing PCL Injuries
While it’s impossible to prevent all injuries, certain measures can reduce the risk of PCL injuries:
- Proper Training: Ensuring correct techniques in sports and exercises.
- Strengthening Exercises: Focusing on leg muscles to support knee stability.
- Protective Gear: Using knee pads in sports and appropriate restraints in vehicles.
ACL vs PCL (Difference between ACL and PCL)
Understanding ACL and PCL in Knee Joints
Location:
- The ACL is located in the center of the knee joint anteriorly, crossing diagonally with the PCL.
- The PCL is located in the center of the knee joint posteriorly, crossing diagonally with the ACL.
Function:
- ACL prevents tibia from sliding forward relative to the femur, providing stability during activities like jumping, landing, and pivoting.
- PCL prevents tibia from sliding backward relative to the femur, maintaining stability during activities like pushing off the ground or decelerating.
Injury Predisposition:
- ACL tears are more common in sports involving sudden stops, changes in direction, and jumping.
- PCL tears are less frequent but can occur from forceful blows or hyperextending the knee.
Symptoms of Injury:
- Both ACL and PCL tears can cause pain, swelling, knee instability, and difficulty walking.
Treatment:
- Mild tears can be treated non-surgically with rest, ice, compression, physical therapy, and bracing.
- Severe ACL and PCL tears often require surgery for reconstruction.
Conclusion
PCL injuries, though less common than ACL injuries, can significantly impact one’s quality of life. Understanding the causes, symptoms, and treatment options empowers individuals to seek timely medical attention and follow effective rehabilitation programs. Whether through non-surgical methods or surgical intervention, the goal is to restore knee function and prevent future injuries. By adopting preventive measures and staying informed, individuals can protect their knees and maintain an active, healthy lifestyle.
References:
- Introduction: https://www.ncbi.nlm.nih.gov/books/NBK430726/
- Symptoms: https://my.clevelandclinic.org/health/diseases/21793-pcl-posterior-cruciate-ligament-tears#symptoms-and-causes
- Causes: https://orthoinfo.aaos.org/en/diseases–conditions/posterior-cruciate-ligament-injuries/
- Diagnosis: https://www.webmd.com/fitness-exercise/posterior-cruciate-ligament-injury
- Treatment: https://orthoinfo.aaos.org/en/diseases–conditions/posterior-cruciate-ligament-injuries/
About Author –







 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

