Liver Transplantation: Current Status and Challenges

Introduction
Over the last several decades, the field of transplantation has witnessed a lot of change. Yet, among all solid organ transplants, arguably the greatest advances have been in liver transplantation. Currently, more than 40 years after the first successful liver transplantation by Dr. Starzl, more than 100,000 liver transmutations have been performed in the world. Advancements in surgical technique, preoperative management, and immunosuppressive therapy have yielded excellent graph and patient survival outcomes which have become the expected norm.
Types of Liver Failure
Today, liver transplantation is universally accepted as the only definitive treatment for end-stage liver disease, acute fulminant hepatic failure, hepatocellular carcinoma, and several metabolic disorders. Prior to the advent of liver transplantation, the only treatment options available to patients with end stage liver disease (acute liver failure or cirrhosis) were symptomatic in nature and devoid of curative ability.
Acute Liver Failure
Acute liver failure (ALF) is a critical medical condition defined as rapid development of hepatic dysfunction associated with encephalopathy. The etiology of ALF in India shows some variation from the West. For example, in some series, ALF has been most commonly been due to viral hepatitis followed by drug injury due to anti-tubercular therapy. On the other hand cases of paracetamol poisoning, which is one of the commonest causes in the West, do not make up a significant number of ALF patients in India.
Liver transplantation is performed for patients with ALF who are unlikely to respond to medical management. ALF accounts for 8% of indications for liver transplantation. Current liver transplant results are especially good considering the emergency context of the surgical indication, with one and five-year patient survival rates of 80% and 75% respectively.
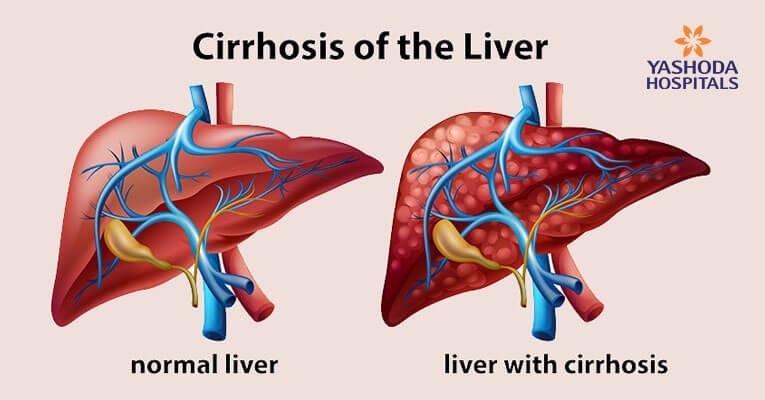
Liver Cirrhosis
The most common indication for liver transplantation is cirrhosis of the liver. Cirrhosis is the 11th leading cause of death worldwide. It is the end result of many chronic liver diseases, the most common being viral hepatitis, alcoholic liver disease, and non-alcoholic fatty liver disease. Liver cirrhosis has many other causes, including inherited diseases such as hemochromatosis and Wilson’s disease, primary Biliary cirrhosis, primary sclerosing cholangitis, and autoimmune hepatitis. Some cases are idiopathic or cryptogenic. It occurs when repeated hepatocyte damage results in the formation of fibrous tissue and the development of regenerative nodules.
Although the causes of liver cirrhosis are multi-factorial, there are some pathological characteristics that are common to all cases of liver cirrhosis, including degeneration and necrosis of hepatocyte, and replacement of liver parenchyma by fibrotic tissues and regenerative nodules, and loss of liver function.
Chronic liver disease passes through several stages before it reaches the irreversible end stage. Fibrosis as a precursor of cirrhosis is a pivotal pathological process in the evolution of all chronic liver diseases to cirrhosis. Removing the etiological factors is the most direct and perhaps most effective method of treating liver fibrosis.
As such, treatments against HBV and HCV infections, abstinence from alcohol abuse, weight, and blood lipid control, chelation of overloaded iron and copper are considered potentially effective therapies for a large proportion of liver fibrosis cases. Unfortunately, the phases of chronic liver disease that precede liver cirrhosis are usually asymptomatic and hence remain untreated in a large proportion of patients.
The natural history of cirrhosis is characterized by a silent, asymptomatic course until increasing portal pressure and worsening liver function produce a clinical phenotype, called ‘‘decompensated cirrhosis”. In the asymptomatic phase of the disease, usually referred to as “compensated cirrhosis”, patients may have a good quality of life, and the disease may progress undetected for several years. Decompensation is marked by the development of overt clinical signs, the most frequent of which are ascites, bleeding, encephalopathy, and jaundice. Following the first appearance of any of these, the disease usually progresses more rapidly towards death or liver transplantation.
The transition from compensated asymptomatic cirrhosis to decompensated cirrhosis occurs at a rate of about 5% to 7% per year. Once decompensation has occurred, cirrhosis becomes a systemic disease, with multi-organ/system dysfunction. At this stage, patients become highly susceptible to bacterial infections because of complex cirrhosis-associated immune dysfunction, which involves both innate and acquired immunity. In turn, patients with bacterial infections are burdened by severe morbidity and high mortality. Because of these events, decompensation represents a prognostic watershed, as the median survival drops from more than 12 years for compensated cirrhosis to about two years for decompensated cirrhosis without liver transplantation.
Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC) is the fifth most common cancer and the second most frequent cause of cancerrelated death globally. It is the most common primary liver cancer and most patients with HCC also suffer from coexisting cirrhosis. For the treatment of patients without cirrhosis, resection should be considered whenever possible. The hepatic reserve is one of the major determinants for liver resection. When compared with resection, transplantation restores liver function and has the advantage of removing tissue with oncogenic potential. Liver transplantation is recommended as the first-line option for HCC, which are unsuitable for resection.
Milan’s criteria serve as the benchmark for selection of patients with HCC who can benefit most from liver transplantation. Patients with solitary tumor of less than 5 cm and those who have up to 3 tumor nodules each of which is smaller than 3 cm without vascular invasion or extrahepatic metastas were found to achieve 4-year survival rates of 75%.
Conceptually, the indication for liver transplant embraces two simple criteria. First, the patient should have irreversible and otherwise incurable acute or chronic liver disease. Second, a longer life should be predicted with a transplant than in its absence, a concept referred to as transplant survival benefit.
Types of Liver Transplantation
Living Donor Liver Transplantation
Due to the scarcity of cadaveric donor organs, healthy relatives of the patient come forward as organ donors. Living Donor Liver Transplantation(LDLT) is currently the most effective alternative to overcome the organ shortage in adults. A part of the donor’s liver is harvested for transplantation into the recipient. The reduced waiting period for a living donor organ may decrease the risks of decompensation or death before transplantation, thereby improving the overall chances for success. The main advantage of LDLT over DDLT is that the quality of the graft can be ensured with more certainty in LDLT than in DDLT. As both the donor and recipient operations can be performed simultaneously, the graft ischemia times can be lessened. Disadvantages are the risk to healthy donors. Also, the surgical procedures for LDLT are technically more challenging.
Adult to adult LDLT requires transplantation of the right lobe of the donor into the recipient. This requires harvesting of the right lobe graft without the middle hepatic vein (MHV), but with fastidious preservation of its tributaries. The MHV is retained on the donor side for improved outflow of the residual liver. The preserved MHV tributaries are reconstructed in the back bench before implantation into the recipient. Unlike DDLT, where the common hepatic duct is available for anastomosis, in LDLT, small stump(s) of the right hepatic duct are anastomosed requiring meticulous attention to ductal vasculature to prevent Biliary stricture/ leak.
A graft from a living donor provides excellent function because of the short Ischemic time and the lack of adverse factors found in cadaveric donors. Due to the elective nature of the operation and the choice of undergoing the transplant at an early stage of disease, instead of deteriorating while in the waiting list for a cadaver organ, the results of LDLT have improved to more than 95% short-term survival.
Deceased Donor Liver Transplant
Deceased Donor (Cadaveric) Liver Transplant(DDLT) is the most common form of liver transplantation done worldwide. For Deceased donor liver transplantation, the patient registers as a potential organ recipient in the state’s organ distribution network, Jeevandan in the case of Telangana. Whenever an organ gets allocated to the patient, he can undergo liver transplantation.
The cirrhotic liver is removed (explanted) and the donated organ is transplanted in its place- orthotopic liver transplantation. The cirrhotic patient is sicker than the conventional patient undergoing surgery, he tends to be coagulopathic with raised INR, low platelet count, and scanty antifibrinolytic factors. The portal hypertension results in an increased chance of bleeding due to the extensive dilated collateral, posing both serious surgical and anesthetic challenges. After implantation of the graft, there is the risk of reperfusion injuries. Also, the anastomoses of the hepatic veins, portal vein, the small calibrated hepatic artery, and bile ducts require meticulous surgical techniques backed by experience to perform.
Liver Transplantation In India
Liver transplantation arrived in India many decades after it was successfully performed in the developed world. The last few years have seen an exponential rise in the number of liver transplants done in India. India has now emerged as the regional transplant center for South East Asia. About 25% to 30% of the total transplants per year are performed on patients from other countries. The liver disease burden in India is quite large with 22.2 deaths per 100,000 population attributed to cirrhosis by the Global Health Observatory data from the World Health Organization (WHO). It has been estimated, very conservatively, that approximately 20,000 patients require a liver transplant in India annually. Yet only around 800-1000 liver transplants are currently performed every year on Indian patients.
Two main obstacles remain for patients requiring a liver transplant in not getting one. First is the cost. Though liver transplantation is being performed in India for a fraction of its cost in the developed world, it is still one of the most expensive treatment modalities. Second is donor availability. The patient has the option of waiting for a cadaveric organ donation to undergo. Deceased Donor Liver Transplantation (DDLT) or to undergo Living Donor Liver Transplantation (LDLT) utilizing a partial liver graft donated by one of his relatives.
Conclusion
There is a large discrepancy between the number of patients requiring a liver transplant and the number of transplants being done in our country. With expertise available for both LDLT and DDLT, many of these patients can be offered a definitive treatment for their lethal liver disease. Early referral for liver transplantation will help the patient to explore both options and choose the appropriate treatment modality.
















 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More