Fatty Liver Disease: Symptoms, Causes, Risks, and Treatment
Fatty liver disease has definitely caught on as a health concern for numerous individuals across the globe. It happens when there is an accumulation of excess fat in the liver, which may eventually result in a number of serious problems. Although it is usually asymptomatic at first, in some cases it can end up causing liver inflammation, scarring, and even total failure. Consequently, there are exceptional benefits to understanding its causes, signs, and prevention strategies in the early days in order to protect liver health.
What is a Fatty Liver Disease?
Fatty liver disease (FLD), also called hepatic steatosis, is a health condition characterized by the accumulation of too much fat in the liver. The liver is an organ that processes nutrients and filters out harmful substances. Excess fat intake can lead to liver inflammation, resulting in liver injury or scarring, which may finally lead to liver failure in some cases. In most cases, fatty liver disease (FLD) exhibits chemicals without any clinical symptoms. As time progresses, fat accumulation makes it difficult for the liver to perform its functions; therefore, there are risks of possible health issues.
Fatty liver disease can also be called alcoholic fatty liver disease, alcoholic steatohepatitis, nonalcoholic fatty liver disease (NAFLD), or nonalcoholic steatohepatitis (NASH) based on its severity. The new terminology for NAFLD is MASLD (metabolic dysfunction-associated steatotic liver disease).
Excessive alcohol consumption leads to alcoholic fatty liver disease, which is one of the major liver diseases, and alcoholic steatohepatitis, which is a severe form with inflammation. Non-alcoholic fatty liver disease (NAFLD), the leading type of liver disease that does not result from alcohol intake, and nonalcoholic steatohepatitis are serious variants of NAFLD associated with inflammation and liver damage.
Types and Stages of Fatty Liver Disease
Types of fatty liver disease
Fatty liver disease is of mainly two types: alcoholic fatty liver disease and nonalcoholic fatty liver disease. Apart from these, there is an uncommon type that especially occurs during pregnancy, known as acute fatty liver of pregnancy.
Nonalcoholic fatty liver disease (NAFLD):
People who do not consume, in any way or little, alcohol experience NAFLD, which occurs when there is excessive fat accumulation in their livers. This type of NAFLD, which does not have a strong alcohol use history, is termed simple NAFLD. NAFLD, also sometimes referred to as NASH, involves a condition whereby fat accumulates in the liver, leading to inflammation.
There is a move to change the terminology of non-alcoholic fatty liver disease (NAFLD) to metabolic dysfunction-associated steatotic liver disease (MASLD) due to the main cause. Experts also suggest replacing the term non-alcoholic steatohepatitis (NASH) with metabolic dysfunction-associated steatohepatitis (MASH). This NAFLD can be diagnosed based on these three criteria: excess fat deposits, an inflamed liver, and no past consumption of heavy alcohols. If NASH is left untreated, it may lead to liver fibrosis, cirrhosis, and failure.
Alcoholic fatty liver disease (AFLD):
This is the initial phase of alcohol-associated liver impairment. Alcoholic steatohepatitis (ASH) is a grave variety of AFLD characterized by excessive fat accumulation and an inflammatory response. ASH is diagnosed by a doctor if there is excess fat, inflammation, and too much alcohol consumption. If not treated properly, ASH may progress towards liver cirrhosis as well as severe liver scarring, which could result in hepatic failure.
Acute fatty liver of pregnancy (AFLP):
AFLP is a rare pregnancy complication characterized by excessive fat accumulation in the liver. It usually occurs during the third trimester and has serious health implications for both the mother and the child. The diagnosis needs delivery as well as postnatal follow-up care.
Stages of fatty liver disease
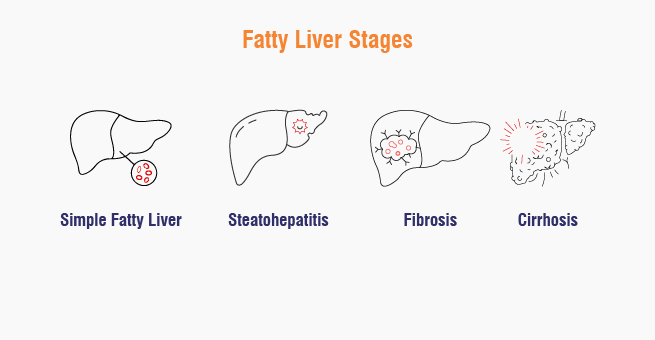
Fatty liver is of mainly four stages:
1. Simple Fatty Liver: An accumulation of fat (too much fat) in the liver that does not usually cause any problems.
2. Steatohepatitis: Inflammation of the liver together with fat in excess.
3. Fibrosis: Continuous inflammation leads to scars formed in the liver, hampering its normal functions.
4. Cirrhosis: A widespread liver scarring that interferes with functioning organs, making it irreversible, and this is considered an advanced stage.
AFLD and NAFLD are similar, but the causative factor defines the type. Often, a fatty liver causes no noticeable symptoms but may cause fatigue, discomfort, or abdominal pain in some cases. Cirrhosis-related liver damage is permanent, so prevention is very crucial in those cases.
Symptoms, Causes, and Risk Factors of Fatty Liver Disease
Fatty liver symptoms
ALD and NALD typically have no symptoms, but some may experience fatigue or abdominal pain. AFLD and NAFLD present similarly, but fatty liver damage can cause no noticeable symptoms. However, steatohepatitis or cirrhosis may show symptoms such as:
- Pain in the right upper quadrant of the abdomen
- Sluggishness or tiredness
- No desire for food
- Fluid buildup in the tummy (ascites)
- Decrease in weight
- Feeling sick
- Skin with irritants
- Urine that is darkened
- Pale-colored stools
- Yellow coloration of the skin and eyes
- Bruises or bleeding easily
- Swelling (edema, specifically in the legs)
- Growth of mammary glands among men
- Confusion
- Web-like masses formed from blood vessels below the epidermis
Note : These symptoms are not shown by everyone; they may appear in some people, and in others, the condition can be revealed through confirmatory tests.
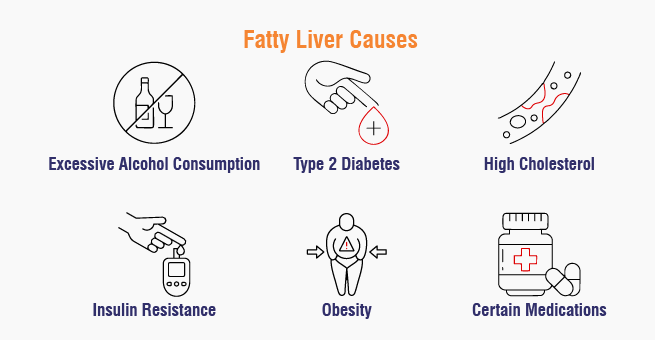
Fatty liver causes
Alcoholic fatty liver disease (AFLD) is caused by excess fat accumulation in liver cells, primarily due to excessive alcohol consumption. This accumulation can lead to the formation of fat types that accumulate in the liver. In contrast, individuals who don’t consume excessive alcohol may have increased fat production or an inadequate fat metabolism.
Some of the common causes for non-alcoholics are:
- Overweight
- Type 2 diabetes
- Insulin resistance
- A high level of fat in the blood, mainly triglycerides
- Metabolic disease conditions
In addition to the above causes, some of the possible reasons for fatty liver include pregnancy, certain medications that can cause adverse effects, certain infections, which include hepatitis C, rapid weight loss with excessive fasting, and some specific, rare hereditary disorders.
Fatty liver disease risk factors
In general, the fatty liver is influenced by several risk factors and is categorized based on the types of fatty liver. The common risk factors for fatty liver disease include:
- Heavy alcohol consumption, defined as 15 or more drinks per week for males and 8 or more drinks per week for females, is the main risk factor for AFLD, with research showing that individuals consuming 40–80 grams of alcohol per day over 10 to 12 years are at a higher risk.
- Advanced age, genetic predisposition, being overweight, tobacco use, and previous exposure to certain infections, including type C hepatitis, also act as additional risk factors for AFLD.
Similarly, the risk factors for nonalcoholic fatty liver disease include:
- History of toxins exposure.
- Family history of liver disease and obstructive sleeping apnea.
- Older age as a risk factor.
- Polycystic ovary syndrome.
- Sudden weight loss.
- Certain medications.
- Metabolic disorders.
- High cholesterol levels.
- Rarer genetic disorders like Wilson’s disease, hypobetalipoproteinemia, and more.
Experiencing fatty liver symptoms?
Fatty Liver Complications
The biggest complication for all of these diseases is cirrhosis. As more tissues are inflamed, they grow larger and ultimately affect the functioning of the liver. Some of the common complications of fatty liver disease include:
- Abdominal swelling
- Ascites
- Oesophageal varices that can rupture and bleed
- Confusion and loss of alertness
- Spleen at high activity levels
- Liver insufficiency
- Liver carcinoma
Fatty Liver Diagnosis
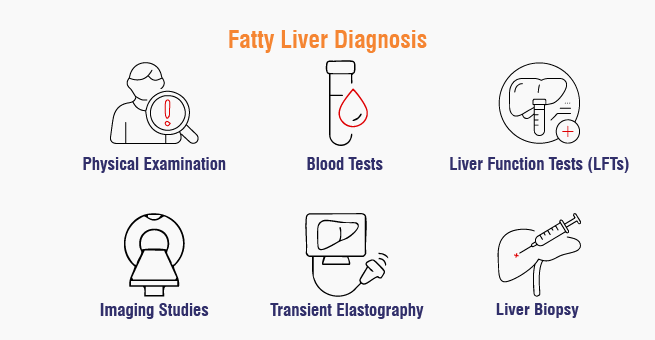
To reach a diagnosis of fatty liver disease, the doctor resorts to the patient’s medical history, physically examines him or her, and then orders tests on him or her. Among others, they may inquire about family medical history, lifestyle patterns, underlying illnesses, or use of drugs, as well as any health changes they have experienced lately.
After that, they used to go for the following tests based on the patient’s requirements:
- A physical examination
- Blood tests such as CBC, LFT, and fasting lipid profile.
- Imaging studies like ultrasound, CT, and MRI examine fat deposits and tissues affected by liver ailments.
- Liver fibroscan, or transient elastography, is performed using non-invasive methods to examine liver stiffness and fat changes in the organ. It can be useful for evaluating individuals who suffer from fatty liver disease; it helps in determining if they are experiencing deterioration of their liver functions. It also quantifies the amount of fat in the liver. Fibrosan is an advanced test that involves placing a small ultrasound probe over the skin over the right ribs and passing a 50-MHz wave into the liver.
- Liver biopsy, involving needle puncture and tissue extraction for laboratory analysis.
Have a medical concern that’s worrying you?
Fatty Liver Treatment
- Usually, there is no direct treatment or medication for the fatty liver. The first line of treatment for the fatty liver includes weight loss, the use of medications for diabetes, cholesterol, blood pressure, and metaboloic disorders, alcohol avoidance, a healthy diet, and maintaining a healthy lifestyle.
- If the person experiences severe liver cirrhosis or liver failure, then he or she might be suggested for a liver transplant.
Lifestyle changes for fatty liver
The doctor might suggest doing the following:
- Increase daily physical activity to at least 60 minutes.
- Prioritize liver health by avoiding alcohol and taking prescribed medications.
- Consult a doctor before trying any remedies.
- Maintain healthy cholesterol levels through a plant-based diet, exercise, and medication.
- Manage diabetes by monitoring blood sugar levels and taking prescribed medications.
- Follow a fatty liver disease diet to reduce or reverse fatty liver disease.
- Limit high-fat foods, replace saturated fats with unsaturated ones, and consume low-glycemic foods.
- Obtaining vaccinations for hepatitis A and B, flu, and pneumococcal disease to prevent liver failure and infections.
- Avoid foods and drinks high in simple sugars.
When to Seek Help from a Doctor
One should visit the doctor if they have any of the following symptoms of fatty liver disease:
- Constant fatigue
- Loss of appetite
- Weight loss
- Nausea and vomiting
- Abdominal pain
- Jaundice
- Dark urine
- Light-colored stools
Early diagnosis and treatment can help prevent complications such as liver cirrhosis and liver cancer.
Experiencing fatty liver symptoms?
Conclusion
Fatty liver disease is a serious condition that can be managed with proper diagnosis and treatment. Yashoda Hospitals in Hyderabad is a trusted and top-rated hospital for liver disease cures and transplants. Skilled doctors and advanced technologies ensure successful results. Early detection and consistent medical care are crucial to preventing the progression to severe liver damage.
Have any questions or concerns about your health? We’re here to help! Call us at +919513262681for expert advice and support.
References:
- Fatty liver: https://www.nhs.uk/conditions/non-alcoholic-fatty-liver-disease/
- Types and stages: https://www.healthline.com/health/fatty-liver#symptoms
- Symptoms and causes: https://www.webmd.com/hepatitis/fatty-liver-disease
- Complications & prevention: https://www.mayoclinic.org/diseases-conditions/nonalcoholic-fatty-liver-disease/symptoms-causes/syc-20354567
About Author –











 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

