Navigating Epilepsy: A Comprehensive Guide
Epilepsy is a neurological condition that results in frequent seizures. It impacts a great number of people across the globe. These seizures are due to the excessive electrical activities occurring within the central nervous system and may range from a loss of slight concentration to major muscle shaking. Whatever it is, understanding the disease in depth, its consequences, and most importantly, the treatment options are crucial in everyone’s life.
What is Epilepsy?
Epilepsy, which is also called seizure disorder, is a brain condition that causes repeated seizures by abnormal electrical signals produced by damaged cells within the brain. Different types of epilepsy exist; some can be identified by a specific cause, and others have no known cause. The changes in awareness, muscle control, sensations, emotions, and behavior result from the seizures caused by damaged cells in the brain.
Many neurons send the signals at a time during a seizure, which is much more rapid than the usual activity. Such a burst of excessive electrical activity might cause involuntary movements, sensations, emotions, and/or behaviors. Loss of consciousness might result from the interference of normal nerve cell activity. In most people, consciousness is restored immediately after a seizure; in others, consciousness returns within minutes or hours. In this intermediate period, the person often feels fatigue, drowsiness, weakness, and confusion.
Epilepsy disease affects more than 50 million people around the world and ranges from brief lapses of attention to severe convulsions. The frequency of seizures can range from fewer than one per year to several per day. In theory, proper diagnosis and treatment could free up 70% of the people suffering from epilepsy.
Epilepsy & Seizures Types
Types of Epilepsy
Epilepsy syndromes are a diverse group of disorders characterized by seizures, which are a prominent symptom. Some of them may be hereditary or even caused by gene changes, while others are unknown. Symptoms or brain origin are the reasons why these syndromes are identified. The types of epilepsy are
- Absence epilepsy is the condition that gives rise to repeated seizures and momentary lapses in consciousness due to a certain disorder, often beginning at ages ranging between childhood and early adolescence or even as family origin factors. Sometimes these seizures cause no apparent symptoms. The episodes can vary from jerky arms to stares into nothingness. Their seizures might be so frequent as to disturb concentration at situations.
- Temporal lobe epilepsy (TLE) is the most common form of epilepsy syndrome, characterized by focal seizures that often occur with nausea, emotions, or an unusual smell or taste. Onset seizures usually begin during childhood or teenage years, with manifestations of staring spells, dream-like states, or repeated automatisms. Repeated TLE seizures cause shrinkage and scarring of the hippocampus, which is very important in memory and learning.
- Frontal lobe epilepsy was found to be a form of epilepsy syndrome where brief focal seizures occur in clusters that target the movement-control region of the brain, which may give rise to muscle weakness or unusual movement and loss of awareness. The seizure was commonly reported to happen either when a person is asleep or awake.
- Neocortical epilepsy is a condition wherein fits originate from the cerebral cortex of the brain. It involves unusual sensations, visual hallucinations, changes in moods, muscle contractions, convulsions, and other symptoms that correspond to the source.
Childhood Epilepsy Types
- Infancy-onset epilepsy syndromes include infantile spasms, childhood absence epilepsy, and Lennox-Gastaut syndrome.
- Infantile spasms are clusters of seizures that usually begin before 6 months.
- Childhood absence epilepsy usually stops when a child reaches puberty, but some children continue to have absence seizures into adulthood.
- Lennox-Gastaut syndrome has several types of seizures, including atonic seizures, which cause sudden falls.
- Rasmussen’s encephalitis is a progressive form of epilepsy characterized by chronic inflammation in half the brain.
- Dravet syndrome and Tuberous Sclerosis Complex typically start seizures before age one.
- Hypothalamic hamartoma is a rare form of epilepsy associated with malformations of the hypothalamus at the base of the brain.
- Developmental and epileptic encephalopathy (DEE) is a group of severe epilepsies characterized by drug-resistant seizures and significant developmental delay or loss of skills.
Types of Seizures
Epilepsy, also known as seizures disorder, is usually characterized by a group of recurrent seizures. However, seizures are categorized into focal and generalized types, each with various types within each category.
- Focal seizures
Focal seizures start from one area of the brain. They occur in nearly 60% of those who have epilepsy. Motor, sensory, or psychic feelings, sensations, and abnormal behaviors can be involved. Some have auras: warning of an upcoming seizure, symptoms in the region controlled by the region of the brain. Sometimes focal seizures mimic other diseases; thus, they have to be closely followed with testing. - Generalized seizures
Generalized seizures are caused by abnormal neuronal activity that spreads quickly over both sides of the brain. Such seizures may lead to loss of consciousness, falls, or severe muscle contractions. The types of generalized seizures are:
- Absence seizures: staring blankly, sometimes with twitching of muscles.
- Tonic seizures: stiffening of the back, legs, and arms.
- Clonic seizures: jerking movements of muscles in cycles.
- Myoclonic seizures: jerks or twitches of the upper body, arms, or legs.
- Atonic seizures: loss of normal muscle tone, involuntary head fall.
- Tonic-clonic seizures: symptoms include stiffening, repeated jerks, and loss of consciousness.
- Other types
- Febrile seizures are an illness that affects children, causing a high fever. Children with febrile seizures are often not given antiseizure medications unless they have a family history of epilepsy, signs of nervous system impairment, or have had a prolonged or complicated seizure.
- First seizures can be provoked or unprovoked and do not recur unless there is evidence of brain damage or a family history of epilepsy.
Epilepsy Symptoms
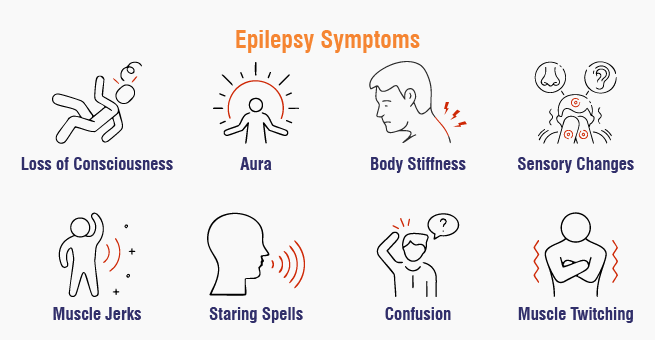
Epilepsy symptoms vary with the specific type of seizure and its intensity, as discussed above. Some of the common symptoms are:
- Aura-unusual sensations, such as strange smells, tastes, or a feeling of deja vu, often precede a seizure.
- Sudden, jerking movements, which cannot be controlled
- Rigidity of the body
- Loss of consciousness
- Epileptic stares
- Disorientation
- Twitching of muscles
- The feeling of tingling or burning
- Change in the perception of smell, taste, or vision
- Problematic speech or even in comprehension
It must be known that not all seizures appear with dramatic convulsions. Some are more subtle and therefore hard to notice.
Experiencing epilepsy symptoms?
Epilepsy Causes
Epilepsy is not contagious. It occurs in people around the world, yet its cause in about 50% of cases remains unknown. Known causes of the disease fall into one of these categories: structural, genetic, infectious, metabolic, and immune. Some of the common causes include:
- Brain damage from prenatal or perinatal causes; for example, a loss of oxygen or trauma at the time of birth.
- Congenital malformations or genetic syndromes with structural anomalies of the brain
- Very severe head injury
- Strokes cutting off oxygen to the brain
- Infection of the central nervous system, like meningitis, encephalitis, or neurocysticercosis
- Some inherited syndromes
- Brain tumors and more
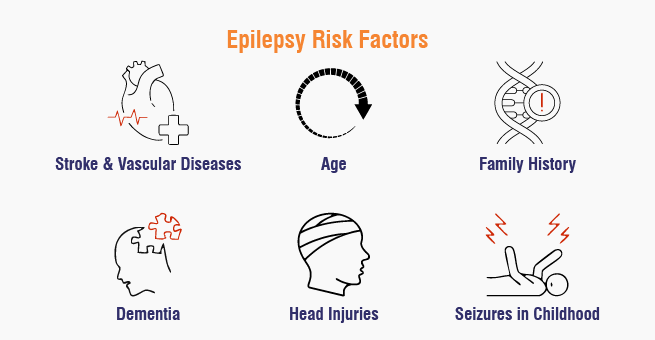
Seizures can be triggered by various environmental factors, including alcohol, flashing lights, illicit drug use, skipping antiseizure doses, lack of sleep, hormone changes during menstruation, stress, dehydration, skipped meals, and illness. While most people with epilepsy don’t have reliable triggers, they often identify factors that make it easier to have a seizure. The following are some of the risk factors that might increase the risk of epilepsy:
- Age: Epilepsy may be common in the pediatric population and geriatrics, but it may appear at any age.
- Family history: Those who have a family history of epilepsy are likely to suffer from seizures.
- Head injuries: One might minimize the risk of acquiring epilepsy if they use seat belts and helmets during such risky activities.
- Stroke and vascular diseases: Preventing alcoholism, smoking, having a healthy diet, and exercise can help reduce the chances of acquiring brain damage and then developing seizures.
- Dementia: Dementia may put a person with old age more at risk for epilepsy.
Brain infections: For example, meningitis: Inflammation in the brain or spinal cord increases the risk - Seizures in childhood: High fevers in early childhood are sometimes associated with seizures, but the risk of epilepsy is higher if a child has a prolonged fever-associated seizure, another nervous system condition, or a family history of epilepsy.
Epilepsy Complications
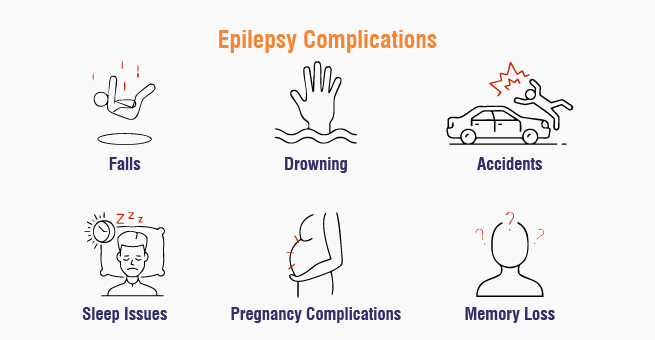
Epilepsy might lead to the following complications in some cases:
- Falls: Seizures can cause head injuries or bone fractures.
- Drowning: Seizures increase the risk of drowning in individuals with epilepsy, especially in water.
- Accidents: Seizures causing loss of awareness or control can lead to accidents.
- Sleep issues: Epilepsy can lead to insomnia.
- Pregnancy complications: Epilepsy during pregnancy can cause birth defects.
- Memory loss: Some epilepsy types can cause memory issues.
Take control of your epilepsy.
Epilepsy Diagnosis
The prompt identification of epilepsy is critical in its management as it determines the treatment regimen that will be used. A series of tests are performed to confirm the diagnosis of epilepsy and to specify the seizure type that the person suffers from. In most cases, epilepsy diagnosis takes place when a person experiences two or more unrelated seizures with a break of 24 hours in between. The following are the diagnostic approaches for epilepsy:
Medical History
- A good history of the patient concerning symptoms and duration of fits is very important to detect epilepsy.
- Past history of illnesses and family history of seizures is also important.
Imaging and Monitoring Techniques
- Electroencephalogram (EEG): Electrical activity of the brain measured. It detects abnormalities, and the requirement of antiseizure drugs is ascertained.
- Stereoelectoencephalograpy (SEEG): surgical implantation of electrodes into the brain for seizure location.
- Magnetoencephalogram (MEG): It measures the magnetic signals produced by neurons that can help in finding some unusual activity in the brain.
- Computerized tomography and magnetic resonance imaging (CT and MRI): It shows structural problems in the brain, for example, tumors and cysts.
- Positron emission tomography (PET): It takes pictures of the brain and shows regions that have normal and abnormal chemical activity.
- Single photon emission computed tomography (SPECT): It finds the site of focal seizures in the brain.
Blood Tests
- Screening for undiagnosed underlying illnesses such as infection, lead poisoning, anemia, and diabetes.
Developmental, neurological, and behavioral tests
- Determine if epilepsy has any effects through measurement of motor skills, behavior, and intellect.
Epilepsy Treatment
Once epilepsy is diagnosed, the patient should take the treatment as soon as possible. There are many ways of successfully controlling seizures. Depending on the individual and the type of epilepsy, there are several approaches to treatment.
- Medications: Epilepsy is commonly treated with antiseizure medications, with over 40 available today. The best drug depends on factors like seizure type, lifestyle, frequency, side effects, and pregnancy. Doctors start with a low dose and adjust as needed. Side effects can worsen over time, so consult with a doctor. Discontinuing medication with supervision is crucial, and some individuals may need surgery, dietary changes, or devices to stop seizures.
- Dietary changes and lifestyle modifications: Epilepsy can be treated with a ketogenic diet, a high-fat, high-protein, low-carbohydrate diet, which induces ketosis, reducing seizures. However, maintaining this diet requires monitoring for nutrient intake and potential kidney stones. Sleep hygiene is also crucial for seizure reduction.
- Surgery: Epilepsy surgery is considered after unsuccessful attempts at medications or a brain lesion is found to cause seizures. Surgery can reduce or stop seizures, but it can cause cognitive or personality changes and physical disability. It is recommended to continue antiseizure medication for at least two years after surgery. Surgical procedures include:
- Multiple subpial transections
- Corpus callosotomies
- Hemispherectomy
- Thermal ablation
- Devices: Some people may use neurostimulation devices to treat their epilepsy. These devices deliver electrical stimulation to the brain to reduce seizure frequency.
- Vagus nerve stimulation is a surgical procedure that involves implanting a device under the chest skin, which delivers short bursts of electrical energy to the brain.
- Responsive stimulation is a method where an implanted device analyzes brain activity patterns to detect a seizure, then administers an intervention to prevent it.
- Deep brain stimulation involves implanting an electrode connected to a pulse generator to deliver electrical stimulation to specific brain areas, regulating neural circuit signals.
Take control of your epilepsy.
When to Seek Medical Attention with a Doctor
One should immediately seek medical care if they have their first seizure or have more than one seizure. Moreover, one should see a doctor in the following instances:
- Seizures are recurring and do not stop.
- Experiencing the change in the pattern of seizures or frequency.
- Identifying the new signs of a seizure or worsening of previous ones.
- When the medication does not control the seizures.
- Experiencing unwanted side effects from the seizure medicines
Early diagnosis and proper treatment by neurologists are the major factors in achieving successful management of epilepsy and improved quality of life.
Conclusion
Living with epilepsy is not easy, but proper diagnosis, treatment, and support can help an individual manage the condition and live a full life. If you or someone you know is experiencing seizures, you should seek medical attention right away.
Yashoda Hospitals renders complete care for the sufferers of epilepsy. Our experienced neurologists and neurosurgeons offer advanced diagnostic tools and effective treatment options to help manage seizures and improve quality of life.
Have any questions or concerns about your health? We’re here to help! Call us at +919513262681 for expert advice and support.








 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

