Comprehensive Guide to Cornea Transplant: Procedure, Recovery, and Long-Term Care
The cornea plays a crucial role in vision, accounting for 65–75% of light refraction while also protecting the eye from foreign objects and UV radiation. Though it can heal from injuries, improper care can lead to complications like scarring or infection, which may impair vision. Regular checkups with an eye specialist and a diet rich in vitamin E found in foods like avocados and almonds help maintain corneal health.
What is a Cornea Transplant?
A cornea transplant surgery, also known as keratoplasty, is a procedure where part of the cornea is replaced with donor tissue. The cornea is the clear, dome-shaped surface of the eye that allows light to enter, playing a vital role in clear vision. A cornea transplant can help restore vision, reduce pain, and improve the appearance of a damaged or diseased cornea. While most transplants are successful, there is a small risk of complications, including rejection of the donor tissue.
Most frequently, a corneal transplant is needed for someone with damaged corneas to regain vision, alleviate discomfort, or other symptoms related to corneal disorders. With a corneal transplant, a variety of disorders can be treated, including keratoconus, where the cornea bulges outward, Fuchs’ dystrophy, a genetic disorder, thinning or tearing of the cornea, scarring from infection or injury, swelling, corneal ulcers unresponsive to treatment, and complications from previous eye surgeries.
Why does Cornea Rejection Occur?
Cornea rejection occurs when the immune system mistakenly attacks the donor cornea, potentially requiring medical intervention or another transplant. Urgently consult your eye doctor if you experience symptoms such as vision loss, eye pain, redness, or sensitivity to light. Rejection affects about 10% of cornea transplant cases.
Corneas used in transplants come from deceased donors, but not from those who died from unknown causes or had previous eye surgeries, eye diseases, or certain transmissible conditions. Unlike organ transplants, such as liver or kidney transplants, cornea transplants do not require tissue matching.
Need clarity on the cornea transplant procedure?
Before and After Cornea Transplant
Before cornea transplant surgery, the following steps are taken:
- A thorough eye exam to identify conditions that could cause complications post-surgery.
- Measurements of the eye to determine the appropriate donor cornea size.
- A review of medications and supplements to identify any that may need to be stopped before or after surgery.
- Treatment of unrelated eye issues, such as infections or swelling, to improve the chances of a successful transplant.
A cornea transplant involves removing either the entire thickness or part of the diseased cornea and replacing it with healthy donor tissue. The cornea surgeon will choose the appropriate method, which may include:
- Penetrating Keratoplasty: A full-thickness transplant where the surgeon removes a small disk of corneal tissue and replaces it with donor tissue, secured with stitches that may be removed later.
- Endothelial Keratoplasty: This removes diseased tissue from the back layers of the cornea, including the endothelium and Descemet membrane. Two types of procedures are:
- Descemet Stripping Endothelial Keratoplasty (DSEK): Replaces up to one-third of the cornea with donor tissue.
- Descemet Membrane Endothelial Keratoplasty (DMEK): Uses a thinner and more fragile layer of donor tissue, making the procedure more challenging but commonly performed.
- Anterior Lamellar Keratoplasty (ALK): Removes diseased tissue from the front corneal layers but leaves the back endothelial layer intact. Depending on the depth of damage, the procedure may be:
- Superficial Anterior Lamellar Keratoplasty (SALK): Replaces only the front layers, leaving the stroma and endothelium intact.
- Deep Anterior Lamellar Keratoplasty (DALK): Used when the damage extends deeper into the stroma, with donor tissue grafted to replace the removed portion.
- Artificial Cornea Transplant (Keratoprosthesis): For patients not eligible for a donor cornea transplant, an artificial cornea may be implanted.
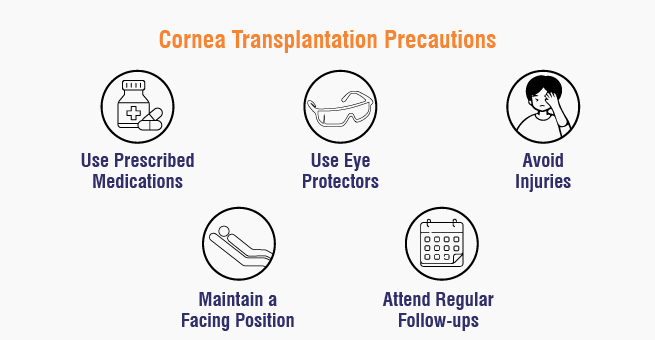
After your cornea transplant, there is a need to follow some precautions. A few important precautions include:
- Medications: Eye drops and other medicines will help control infection, swelling, and pain, including immune-suppressing drops to prevent rejection.
- Eye protection: Use eye shields or glasses to protect your eye as it heals.
- Maintain a face-up position: Depending on the type of transplant, staying on your back for a period after surgery helps the new corneal tissue settle properly.
- Avoid injury: Take it easy after the transplant and slowly resume regular activities as approved by your surgeon. Avoid rubbing or pressing the eyes, and take precautions to protect the eye for life.
- Attend regular follow-up appointments: Regular check-ups with an ophthalmologist in the first year are essential to monitor recovery and detect complications.
What to Expect After the Surgery?
Most people who undergo a cornea transplant will experience corneal restoration of their vision. However, the risk of complications, including cornea rejection, remains for years, making annual consultations with an eye doctor essential. Fortunately, corneal rejection can often be managed with medication.
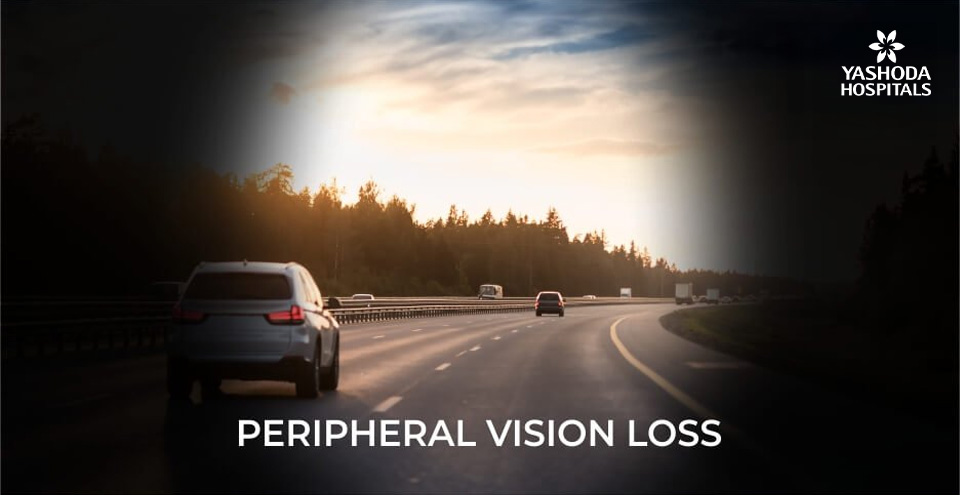
Vision improvement takes time, with several months needed for the eye to fully adjust to the new cornea. It may take weeks to months for the outer layer of the cornea to heal. Once healed, an ophthalmologist can make adjustments to enhance vision, such as:
- Correcting corneal irregularities: Stitches used to secure the donor cornea can create surface unevenness, leading to astigmatism and blurry vision. The doctor may alleviate this by adjusting or removing some stitches.
- Addressing vision issues: Refractive errors like nearsightedness or farsightedness may be corrected with glasses, contact lenses, or, in some cases, laser eye surgery.
Cornea Transplant Recovery Time
The recovery time for a cornea transplant varies based on the type of transplant and individual factors but generally includes several stages. In the first one to three weeks after surgery, it’s crucial to follow postoperative instructions and attend follow-up appointments. Vision recovery can take anywhere from a few weeks to over a year, with possible fluctuations before stabilizing.
Even after vision returns, you may need glasses or contact lenses for optimal clarity. During recovery, activities like swimming and contact sports should be avoided until deemed safe by your surgeon, and it’s important to discuss when it’s safe to resume driving. Consistent follow-up care is essential, and you should contact your doctor if you experience warning signs such as increasing pain, light sensitivity, redness, sudden vision impairment, or ongoing inflammation.








 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

