Role of colon polyps in cancer
At a Glance:
2. What are the symptoms of colon polyps?
3. What are the causes of colon polyps?
4. What are the types of colon polyps?
5. What are the risk factors of colon polyps?
6. How are colon polyps diagnosed by doctors?
7. What are the treatment options for colon polyps?
8. What is polypectomy procedure & its types?
9. What are the risks of polypectomy?
10. Recovery after polypectomy
11. Is polypectomy done at all medical centers or is it done only at specialized centers?
What are colon polyps?
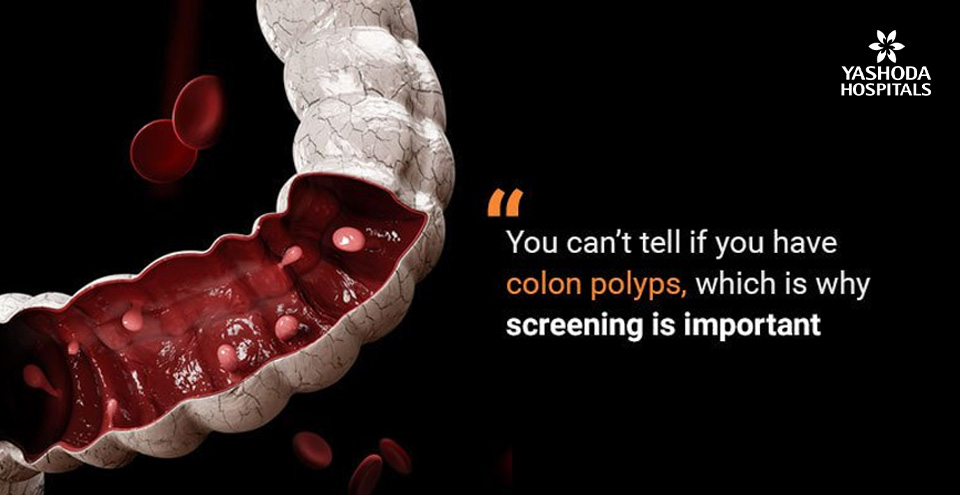
Colon Polyps is a medical condition in which fleshy outgrowths are formed by a clump of cells on the lining of the colon or intestine. In most of the cases, the colon polyps cause no harm, however, some of these polyps may turn into colon cancer, which may even be fatal if not diagnosed in time.
What are the symptoms of colon polyps?
In many cases, colon polyps may not cause any symptoms, and they may get detected only during an examination of the bowel. However, if a person suffers from the following symptoms due to other conditions, colon polyps should be suspected as an underlying cause:
- Bowel habit changes: Constipation or diarrhea lasting for more than a week.
- Change in color of the stools: Stool may present with streaks of blood or may appear black in color.
- Iron deficiency anemia: Prolonged bleeding in stools due to colon polyps may lead to a deficiency of iron and consequently anemia, symptoms of which may be tiredness and shortness of breath.
- Pain: When a polyp of the colon becomes large enough to obstruct the bowel, it may cause abdominal pain accompanied by cramps.
- Bleeding from rectum: Passage of blood from the anus that may be frank or mixed with stool and/or in the form of blood clots.
What are the causes of colon polyps?
Under normal circumstances, cells divide and grow to form tissues and organs at a regular pace and in an organized way. However, certain defects in specific genes may lead to the division of cells even when it is not required. When this unregulated growth takes place in the lining of the rectum or the colon and rectum, it leads to the formation of polyps. The unregulated growth can get triggered due to different causes.
What are the types of colon polyps?
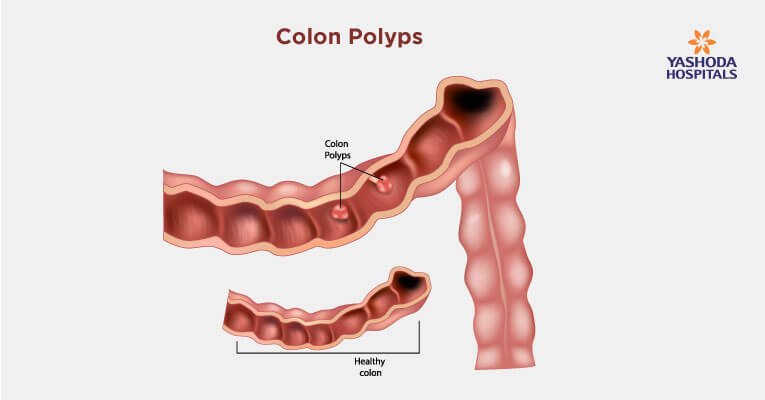
Colon polyps can be categorized on the basis of their shape, on the basis of the pathophysiology of their growth, and on the basis of whether they are cancerous or non-cancerous in nature:
There are two types of polyps on the basis of shape:
- Pedunculated polyps: These are shaped like a mushroom and appear as raised growths. A thin, long stalk or neck known as a peduncle attaches the polyp to the surface or lining of the colon.
- Sessile polyps: These are directly attached to the surface of the colon without a stalk and appear flattened in comparison to pedunculated polyps.
At the microscopic level, the polyps are classified on the basis of their cellular structure and the characteristics of the cells into the following types:
- Inflammatory colon polyps: Chronic inflammatory conditions of the colon trigger the formation of polyps caused due to constant irritation. Medical conditions such as inflammatory bowel disease (IBD), Crohn’s disease, or ulcerative colitis may lead to the formation of polyps in the colon. Such polyps do not usually progress to turn into cancer and are often termed as “false polyps”.
- Hyperplastic polyps: The polyps are formed due to the abnormally fast growth of cells leading to an increase in their numbers, which results in an enlarged growth or polyp. Even though the rate of growth is high, this type of polyps is usually at a low risk of turning cancerous.
- Adenomatous polyps: Also known as adenomas, this type constitutes nearly 70% of colon polyps. It is possible for adenomas to convert into cancers after a prolonged duration, usually years. Adenomas are neoplastic in nature, unlike hyperplasia. This means that they are characterized by “new growth” of cells of an abnormal nature. A mass of neoplastic cells is called a tumor, which can be benign or aggressive i.e malignant.
- Villous adenoma: This is a type of adenomatous polyp with a greater propensity for becoming cancerous. Nearly 30% of villous adenoma eventually turn malignant.
Colon polyps vary in size from very small, usually a few millimeters, to larger ones measuring several centimeters. The size of the polyp may be linked to the probability of becoming cancerous after a certain period of time.
What are the risk factors of colon polyps?
Even though anyone can develop colon polyps, certain categories of individuals are considered to be at a higher risk of developing colon polyps. Some of the factors that may contribute to the formation of colon polyps include:
- Age: In a majority of cases, people diagnosed with colon polyps are 50 years or older.
- Family history: Presence of colon polyps in immediate relatives like a parent, sibling, or a child increases the likelihood of a person to develop colon polyps, more so if many family members have them.
- Inflammatory intestinal conditions: Medical conditions such as Crohn’s disease and ulcerative colitis make a person more susceptible due to changes in the nature of the intestinal lining caused by persistent inflammation.
- Lack of physical exercise and obesity: An unhealthy lifestyle increases the risk of colon polyps as BMI increases.
- Tobacco and alcohol consumption: They increase the risk by promoting harmful changes within the structure of the cells lining the digestive tract.
- Type 2 diabetes: Poorly controlled diabetes increases the risk due to associated hyperinsulinemia and hyperglycemia.
- Hereditary disorders: Some hereditary disorders which are known to be associated with colon polyps include:
- Familial Adenomatous Polyposis (FAP): Polyp formation begins in the teenage years in this condition and may result in thousands of polyps in the lining of the colon.
- Gardner’s syndrome: A variant of FAP that causes polyps to develop throughout the colon and small intestine.
- Lynch syndrome: It is also called hereditary nonpolyposis colorectal cancer.
- MYH-associated polyposis (MAP): A condition similar to FAP that is caused by mutations in the MYH gene.
- Peutz-Jeghers syndrome: A genetic disorder characterized by benign polyps in the gastrointestinal tract. It is usually associated with freckles on the lips, gums, feet, etc. The noncancerous polyps develop throughout the intestines.
- Serrated polyposis syndrome: A condition that leads to multiple serrated adenomatous polyps in the upper part of the colon.
How are colon polyps diagnosed by doctors?
Polyps of the colon are diagnosed by gastroenterologists after taking a thorough medical and personal history of the person followed by examination and performing screening tests that play a key role in diagnosing polyps, more so in situations where they can become cancerous. Some of these screening tests are:
- Colonoscopy: This is a sensitive test for early detection of colon polyps and cancer. In case any polyps are identified during colonoscopy, the gastroenterologist may either remove them immediately or take a piece of tissue (biopsy) for microscopic examination by a pathologist.
- Virtual colonoscopy (CT colonography): A CT scan is used to view the colon in this minimally invasive screening test. If a polyp is identified, colonoscopy is done to remove it.
- Flexible sigmoidoscopy: Examination of the last third portion of the colon (sigmoid and rectum) is carried out using flexible sigmoidoscopy. A slender, lighted tube is inserted through the rectum, and if a polyp is detected, it is removed with a colonoscopy.
- Stool-based tests: This type of test works by checking for the presence of blood in the stool or assessing your stool DNA. If your stool test is positive, you will need a colonoscopy.
- Capsule Endoscopy: A painless procedure in which the person swallows a capsule with an inbuilt camera that takes photographs of the intestine and transmits them. The capsule endoscopy helps in diagnosis and localizing the site of polyps in the colon.

What are the treatment options for colon polyps?
Doctors generally try to remove all polyps that may be discovered during a bowel examination. Some of the techniques for removing polyps are:
- Polypectomy or polyp removal using forceps or a wire loop
- Minimally invasive surgery: Laparoscopic surgery is recommended when the polyps are too large to be removed by colonoscopy or there are safety concerns that prohibit their removal during colonoscopy.
- Colon and rectum removal: Total proctocolectomy or surgical removal of the colon and rectum is recommended in rare cases like Familial adenomatous polyposis (FAP).
What is polypectomy procedure & types?
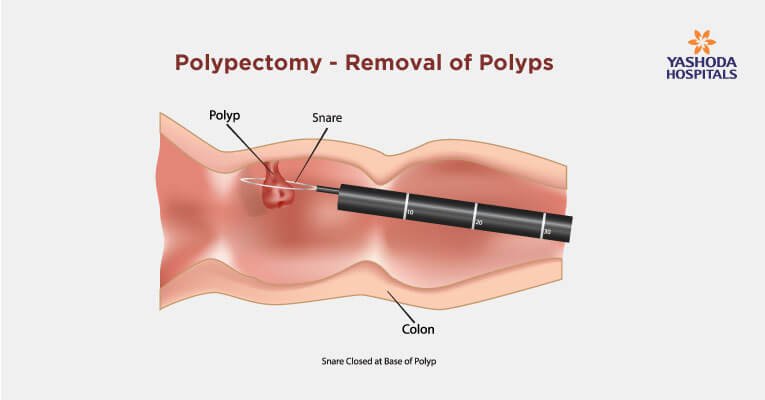
A colonoscopy may be performed for people over 50 years as a screening to check for any potentially cancerous growths or when a doctor recommends the test on the basis of some symptoms. During the colonoscopy procedure, a long, flexible, thin tube (colonoscope) with a camera and a light at the end is inserted into the rectum to visualize the segments of the colon. In case the gastroenterologist who performs the colonoscopy detects the presence of polyps during the procedure, polypectomy i.e. removal of the polyps is performed at the same time. The procedure is relatively non-invasive in nature. Polypectomy can be performed in several ways. The method is usually decided on the basis of what kind of polyps are present in the colon.
- Biopsy forceps removal: For smaller sized polyps that are lesser than 5 millimeters in diameter.
- Snare polypectomy: Polyps that are larger, up to 2 centimeters in diameter, can be removed by this technique. A loop of a thin wire is placed around the bottom of the polyp and the growth is cut off as the wire heats. Any tissue or stalk that remains is cauterized.
- Endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD): This technique is used in more technically challenging cases due to a large size, location, or configuration of the polyp or if there is an increased risk of complications.
- Endoscopic mucosal resection (EMR) or piecemeal resection: A fluid injection made of saline is used to lift the polyp from the underlying tissue before performing the resection or removal of the polyp one piece at a time.
- Endoscopic submucosal dissection (ESD): The fluid is injected deep in the lesion and the removal of the polyp is done in one piece.
After removal, the polyp tissue is sent for pathological examination to assess if it is potentially cancerous.
What are the risks of polypectomy?
Even though it is comparatively less invasive, the polypectomy procedure is not devoid of risk. Some of the risks of polypectomy are:
- Bowel perforation
- Rectal bleeding
The complications of polypectomy are rare, but if the following symptoms are observed after the procedure, the person should immediately consult the gastroenterologist:
- Fever or chills that may indicate an infection
- Unexpected bleeding
- Irregular heartbeat
- Severe abdominal pain or bloating abdomen
- Vomiting
Recovery after polypectomy
Recovery after polypectomy is usually quick and with minor side effects that usually resolve within 24 hours. However, depending on the complexity of the case and the time taken for the procedure, a full recovery can take up to two weeks. Post procedures are advised to the person on self-care.
Driving should be avoided for at least 24 hours, and a person may be asked to avoid certain drinks and foods for 2-3 days that can potentially irritate the digestive system. For example:
- Alcohol
- Coffee
- Soda
- Spicy foods
- Tea
A follow-up colonoscopy is usually recommended to verify the success of the polypectomy procedure by checking that no further polyps have developed.
Is polypectomy done at all medical centers or is it done only at specialized centers?
Polypectomy is a specialized procedure which is recommended to be carried out at specialty centers equipped with comprehensive patient management and diagnostic facilities.
Doctors specializing in gastroenterology and hepatology evaluate and treat colon polyps. Having expertise in different specialties in a single place ensures a multidisciplinary approach to the medical problem. The test results are also available quickly and appointments for different tests and procedures can be scheduled in coordination.
How should one choose a facility for polypectomy?
Choosing the best facility for treatment may be a tough task. Following are some tips for choosing the best facility and treating doctor:
Referrals: Ask your consultant, family members, or friends for the best gastroenterologist in your neighborhood.
Get information: Collect more information about the doctors you have shortlisted. About their experience, education, success rate, and the testimonials of their patients.
Among the several factors accounting for the success of any procedure, the experience and expertise of the treating doctor are most important. The following criteria can be considered while selecting a surgeon:
- He/she should have a master’s degree in gastroenterology or hepatology with experience in the procedure that you may need to undergo. Any advanced fellowships or degrees in this field will add to the credibility.
- He/she should have reasonable experience in performing such procedures.
Hospital Infrastructure: Surgery requires the synchronized efforts of both the doctor and equipment. Get detailed data about the facilities available at the hospital and the experience of the hospital in conducting such procedures.
Each year, doctors at Center for Gastroenterology, Yashoda Hospitals treat hundreds of people for colon polyps, and they also have experience of treating people with rare hereditary polyp disorders like Gardner’s syndrome, juvenile polyposis, Peutz-Jeghers syndrome, etc. The doctors at Center for Gastroenterology, Yashoda Hospitals, make use of the most advanced technology available to not only diagnose colon polyps but also to treat them. During a colonoscopy, to enhance polyp detection, advanced techniques like high-definition narrow band imaging or special staining may also be used. Similarly, the surgeons are committed to using minimally invasive procedures, such as laparoscopy, to treat even very large polyps which may otherwise not be treatable by polypectomy.
Conclusion:
Colon polyps is a medical condition characterized by the formation of fleshy outgrowths in the lining of the large intestine. Even though anyone can develop colon polyps, certain categories of individuals are considered to be at a higher risk of developing colon polyps like those above 50 years of age or with a family history. Symptoms may include bowel habit changes, change in color of the stools, iron deficiency or anemia, abdominal pain accompanied by cramps, etc. Diagnosis of the condition is done through screening tests like a colonoscopy. Treatment options usually depend on the size of the polyp and the structural complexity, which may pose a challenge. Polypectomy, which is a relatively less invasive procedure, is the most preferred technique for smaller size polyps, and those not amenable to polypectomy can be removed laparoscopically. Recovery after polypectomy is usually quick and uneventful.
References:
- Mayo Clinic. Colon Polyps. Available at: https://www.mayoclinic.org/diseases-conditions/colon-polyps/symptoms-causes/syc-20352875. Accessed on June 14th, 2019.
- Harvard Medical School. Colon Polyps. Available at: https://www.health.harvard.edu/a_to_z/colon-polyps-a-to-z. Accessed on June 14th, 2019.
- Medscape. Colon Polyps. Available at: https://emedicine.medscape.com/article/172674-overview. Accessed on June 14th, 2019.
- NIDDKD. Cardiac rehabilitation exercise programme. Available at https://www.niddk.nih.gov/health-information/digestive-diseases/colon-polyps. Accessed on June 14th, 2019.













 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More