Bone Marrow Transplant
In the vast landscape of medical advancements, Bone Marrow Transplant (BMT) stands out as a beacon of hope for individuals facing life-threatening blood diseases. This revolutionary procedure has transformed the treatment landscape, offering new possibilities and improved outcomes for patients dealing with various conditions. Let’s explore the intricacies of BMT, its applications, and the impact it has on the lives of patients.
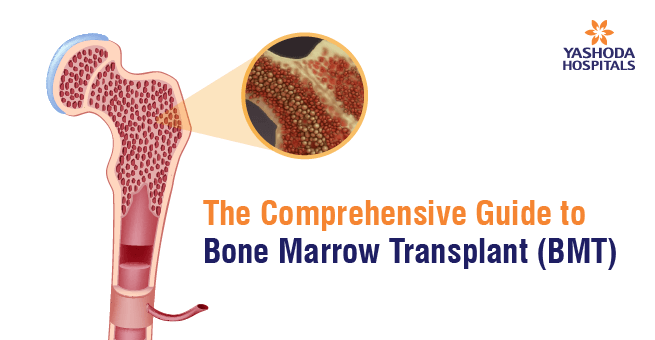
Understanding Bone Marrow Transplant:
Bone marrow, the spongy tissue found within bones, plays a crucial role in the production of blood cells, including red blood cells, white blood cells, and platelets. A bone marrow transplant involves the replacement of damaged or diseased bone marrow with healthy stem cells. These stem cells can be sourced from the patient themselves (autologous transplant), a healthy donor (allogeneic transplant), or umbilical cord blood. The stem cell donor can be an HLA gene-matched sibling or family member or an international donor from the registers.

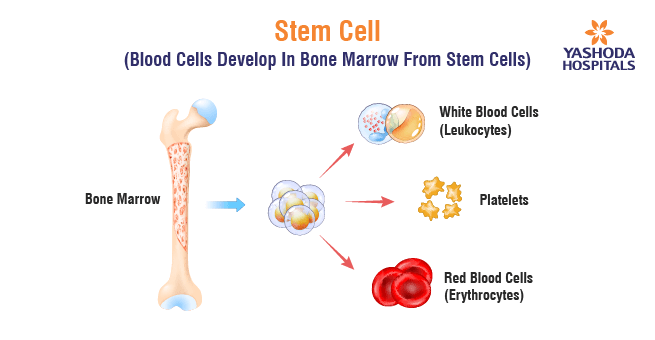
What are Stem Cells?
Stem cells are undifferentiated cells with the remarkable ability to develop into various types of specialized cells. They serve as the body’s internal repair system, capable of dividing and differentiating into specific cell types. In the context of BMT, stem cells play a pivotal role in regenerating the bone marrow and reestablishing the production of healthy blood cells.
Indications for BMT:
The primary purpose of a bone marrow transplant is to treat certain diseases and conditions that affect the bone marrow’s ability to produce blood cells. Here are some common indications for BMT:
- Cancer treatment: BMT is often used in the treatment of various cancers, including leukemia, lymphoma, and multiple myeloma. High-dose chemotherapy or radiation therapy is used to eliminate cancer cells, but these treatments can also damage the healthy bone marrow. A bone marrow transplant helps to restore normal blood cell production.
- Non-cancerous blood disorders: Conditions such as aplastic anemia, thalassemia, and certain types of immune system disorders can lead to insufficient or faulty blood cell production. BMT can be used to replace the defective marrow with healthy donor cells.
- Genetic disorders: Some genetic disorders, like severe combined immunodeficiency (SCID), Wiskott-Aldrich syndrome, and sickle cell disease, may benefit from bone marrow transplantation. The goal is to introduce normal functioning cells to correct the genetic abnormality.
- Autoimmune diseases: In certain autoimmune diseases, where the immune system attacks the body’s own cells, a bone marrow transplant may be considered to reset the immune system and replace it with a healthier one.
- Bone marrow failure syndromes: Diseases like myelodysplastic syndromes (MDS) and myelofibrosis can lead to bone marrow failure, and BMT may be an option to restore normal marrow function.
Types of Transplants and its Applications of BMT:
Types of Transplants:
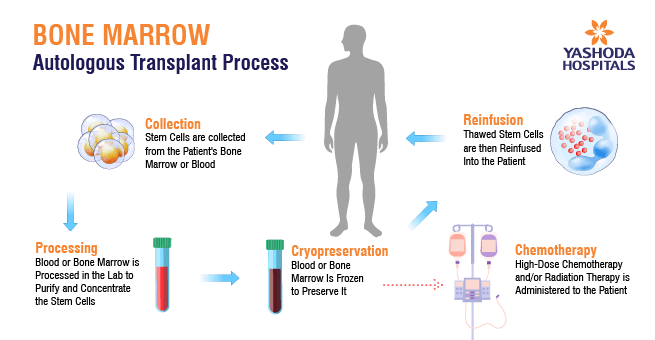
- Autologous Transplant: In an autologous transplant, the patient’s own stem cells are harvested before undergoing high-dose chemotherapy or radiation. After the treatment, the collected healthy stem cells are reintroduced into the patient’s body to aid in the recovery of the damaged bone marrow.
- Allogeneic Transplant: Allogeneic transplants involve the use of stem cells from a compatible donor, which can be a sibling, an unrelated donor, or even a parent. This type of transplant is often used for conditions where the patient’s own stem cells may carry the same genetic abnormalities, as seen in certain hematological and genetic disorders.
- Umbilical Cord Blood Transplant: Stem cells from umbilical cord blood, a rich source of hematopoietic stem cells, can be used for transplantation. This method provides an alternative for patients who do not have a suitable donor.
- Parent-Child Transplant and Haplotype Mismatched Transplant: In certain cases, a parent’s stem cells may be used for transplantation, especially in haplotype mismatched transplants, where the donor is only a half-match. This expands the possibilities for patients who may not find a fully matched donor
How Auto & Allo Transplants Work:
Autologous Transplant:
- Stem cells are harvested from the patient before undergoing high-dose chemotherapy or radiation.
- The collected healthy stem cells are stored.
- The patient undergoes intensive treatment to eliminate diseased cells.
- Stored healthy stem cells are reintroduced into the patient, aiding in the recovery of bone marrow function.
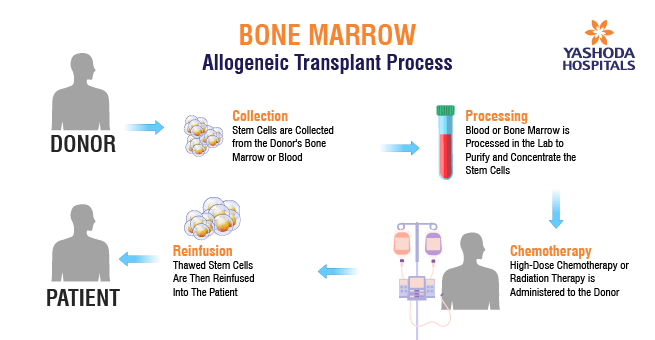
Allogeneic Transplant:
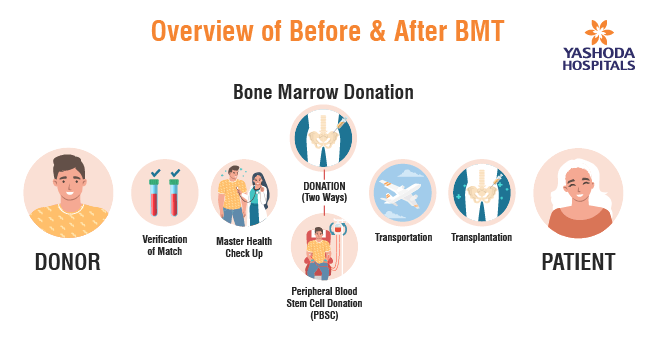
- A compatible donor is identified, often a sibling, unrelated donor, or parent.
- Donor stem cells are collected through bone marrow aspiration or peripheral blood draw.
- The patient undergoes conditioning therapy, which may involve chemotherapy and/or radiation, to prepare the body for the transplant.
- Donor stem cells are infused into the patient, to restore normal blood cell production.
- The immune cells from the donor may attack the remaining cancer cells (graft-versus-tumor effect), but this can lead to graft-versus-host disease (GVHD), where donor cells attack the recipient’s tissues.
Are you aware that smoking causes irreversible lung damage, contributing to 7 million deaths annually worldwide?
The BMT process involves four stages:
The BMT process involves a series of tests to assess a patient’s eligibility and compatibility. These tests include blood tests to evaluate cell counts and detect infections, tissue typing (HLA typing) to determine compatibility with potential donors, crossmatching to prevent immune reactions, imaging studies to assess overall health, bone marrow biopsies to examine the condition of the marrow, and additional tests to evaluate heart and lung function. The BMT tests conducted may vary based on the individual’s health, the reason for the transplant, and the type of transplant being considered. Regular monitoring and assessments are integral to ensure a successful transplantation and post-transplant recovery.
Preparation and Conditioning:
- Evaluate the patient’s health.
- Comprehensive medical assessment, including blood tests, X-rays, and counseling about the procedure.
- Intensive chemotherapy or radiotherapy to destroy diseased marrow.
Harvesting Stem Cells:
- Select a suitable donor (autologous or allogeneic).test
- Collect stem cells from bone marrow, peripheral blood, or umbilical cord blood.
- Administration of stem cells or bone marrow cells with careful management of potential complications.
Transplantation:
- Infuse harvested stem cells into the patient’s bloodstream, isolated in a sterile environment.
- Monitor engraftment, where blood and platelets are transfused, along with antibiotic treatment for infections established in the bone marrow.
Recovery and Follow-Up:
- Provide supportive care during engraftment.
- Monitor for complications and administer post-transplant care.
- Close monitoring of white blood cell count in the initial three months.
- Regular check-ups and frequent blood test
Other Names for BMT : You might hear BMT called by various names, including:
- Allo (Allogeneic) Transplant: Refers to a transplant involving donor cells from another person.
- Auto (Autologous) Transplant: Involves using the patient’s own cells for transplantation.
- BMT (Bone Marrow Transplant): The overarching term for the procedure.
- Haplo (Haploidentical) Transplant: Indicates a half-matched transplant, often involving a parent as the donor.
- HCT (Hematopoietic Cell Transplant): Reflects the transplantation of blood-forming cells.
- SCT (Stem Cell Transplant): Emphasizes the use of stem cells in the procedure.
Challenges, Considerations, and Future
Challenges and Considerations: While BMT offers hope, it is not without challenges. The procedure itself is complex and comes with risks, including graft-versus-host disease (GVHD), where the donor cells attack the recipient’s tissues. Moreover, finding a suitable donor for allogeneic transplants can be a significant hurdle.
Graft-Versus-Host Disease (GVHD):
- GVHD occurs when the donor’s immune cells attack the recipient’s tissues.
- It can lead to various complications, affecting the skin, liver, and digestive tract.
- Prophylactic measures are taken to minimize the risk, but GVHD remains a significant concern.
Finding Suitable Donors:
- Identifying a compatible donor for allogeneic transplants can be challenging.
- Haploidentical transplants have expanded donor options but come with their own set of considerations.
Complex Procedure:
- BMT is a multi-step process involving conditioning therapy, stem cell collection, and transplantation.
- The complexity increases the risk of complications during and after the procedure.
The Future of BMT: Bone Marrow Transplantation (BMT) is characterized by advances in medical research and technology, aiming to enhance the procedure’s efficacy and minimize risks. Ongoing research focuses on reducing graft-versus-host disease (GVHD) through innovative approaches like selective T-cell depletion. Personalized medicine, enabled by genetic profiling, tailors BMT treatments to individual patients, improving success rates and minimizing side effects. Gene therapy, with its potential to correct genetic abnormalities pre-transplantation, holds promise for treating disorders and reducing disease recurrence risk. These developments signal a future for BMT marked by precision, innovation, and personalized therapeutic approaches.
Conclusion: The Bone Marrow Transplant signifies remarkable progress in medical science, offering a lifeline to those battling serious illnesses. Stem cells play a pivotal role in tissue regeneration, showcasing their healing potential. Autologous and allogeneic transplants, addressing a spectrum of disorders, highlight the versatility of BMT. Despite challenges like graft-versus-host disease, ongoing research aims to enhance the procedure’s efficacy through innovative approaches, personalized plans, and gene therapy integration. BMT stands as a beacon of hope, symbolizing healing and renewal amid difficulties, and continues to pave the way for life-saving treatments.
BMT Excellence at Yashoda Hospitals: Pioneering Hematology and Bone Marrow Transplantation in Hyderabad
The Bone Marrow & Stem Cell Transplant Center at Yashoda Cancer Institute in Hyderabad stands at the forefront of excellence in the field of hematology and bone marrow transplantation. Dedicated to advancing hematopoietic stem cell transplant procedures, the center has earned acclaim for its commitment to rare and complex treatments, deploying cutting-edge technology for swift and safe interventions.
Advanced Technology and Skilled Professionals: Yashoda Cancer Institute’s Bone Marrow & Stem Cell Transplant Center is distinguished by its cutting-edge technology and a team of highly skilled professionals. The center’s advanced cell processing laboratory and state-of-the-art facilities uphold the highest standards of safety and efficacy in treatments, with doctors employing innovative therapeutic approaches for optimal patient outcomes.
For the specialized realm of Haploidentical Bone Marrow Transplantation, Yashoda Hospitals goes above and beyond to meet the demanding standards. The Bone Marrow & Stem Cell Transplant Center is equipped with dedicated air handling units, clean rooms, and specialized facilities, ensuring aseptic conditions to prevent infections. A high-quality HVAC system further guarantees complete protection against airborne infections.
In addition to its exceptional infrastructure, the center offers a comprehensive range of diagnostic services. These include 8-color Flow-Cytometry, Minimal Residual Disease detection, molecular diagnosis for leukemia, HLA typing, NK Cell Genotyping, and CD34 + Stem Cell Estimation. The center’s commitment to quality extends to long-term cryopreservation of stem cells and advanced techniques such as Magnetic Separation of Cells using MACS Technology.
Yashoda Hospitals boasts a team of renowned medical professionals specializing in hematology and bone marrow transplantation. Dr. Ganesh Jaishetwar, Dr. K. Karuna Kumar, and Dr. Madhav Danthala, among others, lead the center with their extensive expertise and experience, ensuring top-notch care for patients.
BMT Advancement and Achievements: Yashoda Hospitals is at the forefront of Haploidentical Transplantation, offering a solution when fully matched donors are unavailable. They achieved recognition for performing the first Haploidentical Bone Marrow Transplant in Telangana and Andhra Pradesh. With over 300 completed Bone Marrow Transplants, their expertise spans a wide range of conditions, both malignant and non-malignant.
What sets them apart is a Patient-Centric BMT Process, conducted in four stages with meticulous care, ensuring personalized attention for successful outcomes. In conclusion, Yashoda Hospitals not only marks a milestone in advancing Haploidentical Transplantation but also sets a gold standard in patient-focused Bone Marrow Transplantation. Their journey represents a triumph of medical innovation and compassionate healthcare delivery.
Frequently Asked Questions:
- Why is a Bone Marrow Transplant Needed?
BMT is needed to replace diseased or damaged bone marrow with healthy stem cells, allowing for the production of normal blood cells and immune function.
- Who Can Donate Bone Marrow?
Bone marrow donors can be related or unrelated. Family members, especially siblings, are often preferred, but unrelated donors can be identified through registries.
- Is a bone marrow transplant a painful procedure?
Yes, it can be painful due to the needle insertion, but anesthesia and pain management are utilized for comfort.
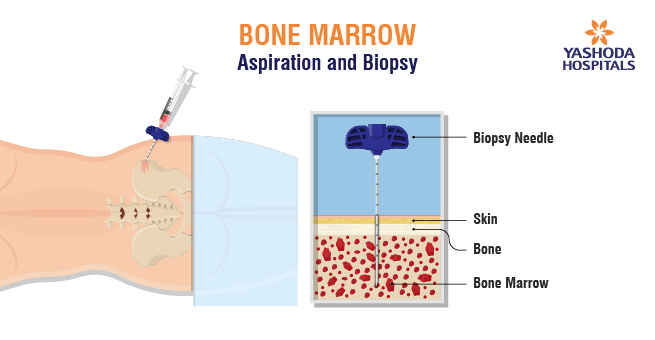
- How is Bone Marrow Collected?
Bone marrow can be collected through bone marrow aspiration, which involves withdrawing liquid marrow from the hipbone, or through peripheral blood stem cell collection, where blood is filtered to collect stem cells.
- What Are the Risks and Complications of BMT?
Risks include infection, graft failure, graft-versus-host disease (GVHD), and side effects from chemotherapy or radiation used in the transplant process.
- What Conditions Can Be Treated with a Bone Marrow Transplant?
Conditions like blood cancer (leukemia, lymphoma, multiple myeloma) and blood disorders such as aplastic anemia, certain genetic disorders, immunodeficiency disorders, and hemoglobinopathies like sickle cell anemia and thalassemia.
- How Long Does the Bone Marrow Transplant Process Take?
The process involves pre-transplant preparation, the transplant itself, and post-transplant recovery, typically spanning several months.
- How Does the Transplant Team Determine Compatibility Between Donor and Recipient?
Compatibility is determined through human leukocyte antigen (HLA) matching. The closer the match, the lower the risk of complications.
- Can Bone Marrow Transplants Be Repeated?
In some cases, a second transplant may be considered if the first one is not successful or if the disease recurs.
- Are There Alternative Treatments to Bone Marrow Transplants?
Depending on the condition, alternative treatments may include chemotherapy, radiation, targeted therapies, or supportive care.
- How Can I Become a Bone Marrow Donor?
Individuals can register with bone marrow donor registries, such as the National Marrow Donor Program (NMDP) or other international registries, to be potential donors.
References:
- https://www.yashodahospitals.com/specialities/hematology-bmt-hospital-in-hyderabad/
- https://www.cancer.net/navigating-cancer-care/how-cancer-treated/bone-marrowstem-cell-transplantation/what-bone-marrow-transplant-stem-cell-transplant
- https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/bone-marrow-transplantation
- https://www.nature.com/articles/s41409-023-02109-x
About Author –
Dr. Ganesh Jaishetwar, Consultant Hematologist, Hemato-Oncologist & Bone Marrow Transplant Physician, Yashoda Hospital, Hyderabad
MD, DM (Clinical Hematology), PDF-BMT (TMC), MACP












 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More