Acute Pancreatitis: Recognizing the Symptoms and Knowing its Causes & Solutions
Acute pancreatitis refers to an inflammatory disease of the pancreas that causes severe complications. The pancreas is a vital organ that yields digestive enzymes; when they become activated in the pancreas, the outcomes could be very lethal or painful. Acute pancreatitis is a complex disease with unclear sources, making it difficult to identify its exact cause. Early diagnosis and timely treatment can avoid complications and improve outcomes. Here’s what you should know about acute pancreatitis—from causes and symptoms to diagnosis and treatment.
1. What is Acute Pancreatitis?
Acute pancreatitis is a serious condition characterized by sudden inflammation of the pancreas within a short period.Pancreas is a small organ located behind the stomach, below the ribcage, which produces digestive enzymes and hormones that regulate glucose metabolism in the body. Most of the people who develop acute pancreatitis have recovered within a week with no complications, but in severe cases, the severity of the cases can bring fatal consequences. Acute pancreatitis is compared with chronic pancreatitis, which experiences a long period of years of inflammation of the pancreas.
Acute pancreatitis typically presents with sudden-onset epigastric pain, which may become sharp and severe, sometimes radiating to the back. Early diagnosis and treatment measures help to improve the patient’s condition and also protect from severe complications.
2. Types of Acute Pancreatitis
The Atlanta classification broadly classifies acute pancreatitis into two categories. These are:
- Interstitial edematous acute pancreatitis, characterized by the acute inflammation of the pancreatic parenchyma and surrounding peri-pancreatic tissue.
- Necrotizing acute pancreatitis, characterized by necrosis of pancreatic parenchyma and peri-pancreatic tissue.
Based on the severity of the disease, acute pancreatitis is divided into the following types:
- Mild acute pancreatitis: In mild acute pancreatitis, there is an absence of local or systemic complications and organ failure.
- Moderate acute pancreatitis: In moderately acute pancreatitis, there are some local complications with or without organic failure for less than 48 hours.
- Severe acute pancreatitis: In severe acute pancreatitis, there is persistent organ failure for more than 48 hours with the involvement of one or more than one organ.
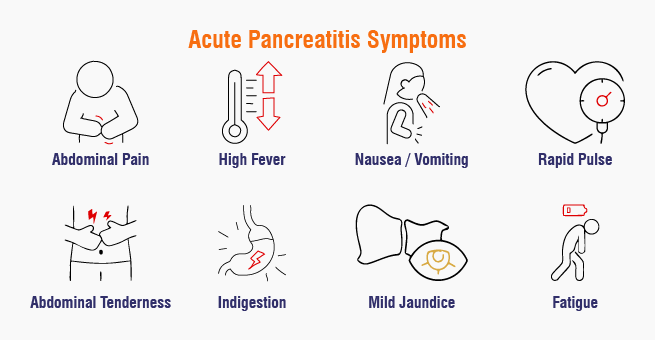
3. Acute Pancreatitis Symptoms
The common signs of acute pancreatitis are sudden and intense abdominal pain in the upper abdomen and high-grade fever. In addition to these, there are some symptoms to watch for, such as:
- Swelling and sensitivity of the stomach
- Vomiting
- Diarrhea (loose stools)
- Nausea
- Rapid heart rate
- Dyspepsia (Indigestion)
- Moderate jaundice
- Fatigue
4. Acute Pancreatitis Causes
The leading causes of acute pancreatitis are the presence of gallstones, overconsumption of alcohol, and excessively high levels of triglycerides in the blood. Gallstones block the bile duct, causing inflammation. Alcohol abuse damages the pancreas, triggering inflammation, and high triglycerides in the blood also trigger inflammation. The prevalence of each cause of acute pancreatitis depends on the geographical region and the social class.
In addition to the above-discussed factors, there are some rare and uncommon factors that might lead to acute pancreatitis, such as:
- Physical injury
- Autoimmune pancreatitis type 1 (Ig4-related systemic disease) and type 2
Coxsackie, Cytomegalovirus, Echovirus, Epstein Barr, Hepatitis viruses A, B, and C, HIV, Mumps, Rubella, and Chickenpox viruses - Structural birth defects—for example, abnormal pancreas that is enveloped
- Hereditary pancreatitis, cystic fibrosis, alpha-1 antitrypsin deficiency
- High calcium levels
- Infections by parasitic agents such as Ascaris lumbricoides, Cryptosporidium, Clonorchis sinensis, and Microsporidia
- Kidney disorders (hemodialysis)
- Toxin substances, including those from scorpion stings and organophosphate poisoning
- Vasculitis syndromes (Polyarteritis nodosa, Systemic lupus erythematosus)
- Pancreatitis as a side effect of medication
- After certain procedures, such as ERCP or any surgical procedure on the abdomen
- Stenosis of the ampulla, which was previously known as schincter oddi dysfunction type
- Proteinacious infections such as Campylobacter jejuni, Legionella, Leptospirosis, Mycobacterium avium complex, and Mycoplasma
- Usage of cigarettes and tobacco products
5. Acute Pancreatitis Diagnosis
The Revised Atlanta classification requires at least two out of three criteria to diagnose acute pancreatitis: a high lipase or amylase level, abdominal pain related to pancreatitis, and abdominal imaging showing suggestive findings. Defining acute pancreatitis involves initial assessment and laboratory evaluations. The diagnostic tests for acute pancreatitis include:
Blood Tests Overview
- Check for high levels of amylase, lipase, blood glucose, and lipids.
- Checks for signs of infection.
Imaging Tests
- Ultrasound, CT scan, magnetic resonance cholangiopancreatography (MRCP), and endoscopic ultrasound are recommended.
6. Acute Pancreatitis Treatment
Acute pancreatitis management depends on the severity of the condition and the patient’s overall health. Treatment of acute pancreatitis may consist of:
- Intravenous fluids or oral rehydration if dehydration is likely.
- Use of analgesic medications for the relief of pain.
- Administration of antibiotics in case of infection.
- Recommended low-fat feeding or alternative means of nutrition through parenteral feeding in more severe cases.
- Ascitic fluid taps out in case there is excessive accumulation of fluid in the abdomen.
- Endoscopic retrograde cholangiopancreatography (ERCP) for the management of the stricture or occluded pancreatic or bile duct.
- Surgery (in severe cases):
– Cholecystectomy: In cases of recurrent acute pancreatitis, removal of the gallbladder may prove valuable.
– Pancreatic Sphincter Sphinteroplasty: This is the procedure that is done with the aim of reconstructing the sphincter muscle of the pancreas.
7. When to Seek Medical Appointment
Out of the many different signs and symptoms that characterize acute pancreatitis, the following are the red flags that should compel you to visit the hospital without any further delay
- Intense pain in the abdomen: It is usually located in the upper part of the stomach and may also be felt at the back.
- Nausea and vomiting: They are common symptoms and usually happen together with a fever.
- Jaundice: A term used to describe the yellowish coloration of the skin and the eyeballs.
- Tachycardia: The pulse rate is above the normal range.
- Abdominal rigidity: The abdomen is likely to be sore on pressure, more so in the upper left area.
In case any of the following symptoms are presented, do not hesitate to take an appointment with the doctor. It could lead to a better outcome in terms of early diagnosis and treatment.
8. Conclusion
Early diagnosis and intervention are crucial for managing acute pancreatitis. Key takeaways include understanding symptoms, causes, and treatment options. Early intervention can prevent complications and improve outcomes.
Yashoda Hospitals in Hyderabad are equipped with advanced medical facilities and state-of-the-art technology to provide comprehensive care for patients with acute pancreatitis. The team of experienced doctors diagnoses and treats the condition effectively, managing complications like fluid imbalances and infections. Yashoda Hospitals also offer advanced treatments like ERCP to address underlying causes.
Have any questions or concerns about your health? We’re here to help! Call us at +918929967127 for expert advice and support.
REFERENCES
- https://www.ncbi.nlm.nih.gov/books/NBK482468/
- https://www.nhsinform.scot/illnesses-and-conditions/stomach-liver-and-gastrointestinal-tract/acute-pancreatitis/#symptoms-of-acute-pancreatitis
- https://www.nhs.uk/conditions/acute-pancreatitis/
- https://www.medicalnewstoday.com/articles/160427#treatments
- https://www.niddk.nih.gov/health-information/digestive-diseases/pancreatitis/symptoms-causes











 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

