Early Signs of Psoriasis: What to Look For and When to Seek Help
Psoriasis, a long-term autoimmune condition that affects millions globally, is a complicated puzzle of skin inflammation and pain. To effectively manage it, understanding its complex mechanisms is the starting point. Knowing its causes, symptoms, forms, and treatments gives one the accessibility to control their skin’s health.
1. What is Psoriasis?
Psoriasis is a chronic skin condition that is caused by an overactive immune response. In normal healthy individuals, skin cells would go through approximately a month’s cycle in regeneration; however, for people suffering from psoriasis, this spans just a few days—in fact, fresh skin cells may surface every 3 or 4 days. This as a result can lead to thick, elevated, red patches that display silvery scales at their tops. These areas may be itchy, painful, sometimes cracking and bleeding, and they can appear all over the body, including the scalp, elbows, knees, and lower back. This disease not only causes physical discomfort but also carries a significant emotional burden, which is often agonizing for individuals, impacting their self-esteem and overall quality of life.
Is Psoriasis Contagious?
Many people believe that psoriasis can be transmitted, but it cannot. Psoriasis is an autoimmune disease. This kind of disease arises when the immune system injures the healthy skin cells by mistake. This overactive immune response causes inflammation and the production of excessive skin cells that manifest clinically as plaques.
2. The Different Types of Psoriasis: A Truly Variable Disease
Psoriasis can therefore show up in different forms, each with a specific set of features:
- Plaque Psoriasis: The most common type, plaque psoriasis exhibits raised, red patches with silver scales.
- Guttate Psoriasis: Small, drop-shaped red lesions, mostly triggered by strep throat.
- Inverse Psoriasis: Red lesions are smooth and present in several skin folds, such as armpits and groins and under breasts.
- Pustular Psoriasis: The presentation of white pustules within red skin can be either localized or generalized.
- Erythrodermic Psoriasis: Seriously widespread red skin and shedding, considered a medical emergency.
- Nail Psoriasis: Involves fingernails and toenails with a pit and thick, discolored, and crumbling appearance.
- Psoriatic Arthritis: The joints have been very painful, stiff, and swollen.
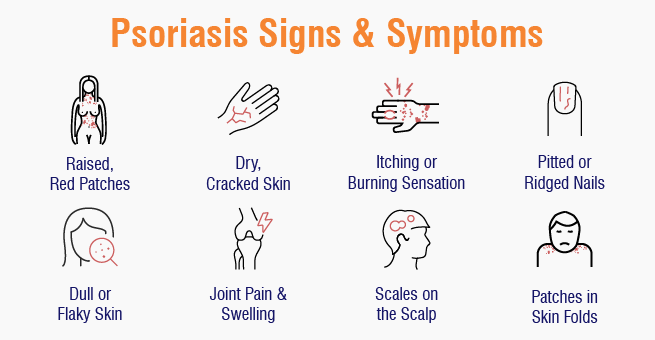
3. Psoriasis Symptoms: Recognizing the Signs
Psoriasis symptoms differ with the type and extent of the condition. Identifying these symptoms is crucial to enabling early diagnosis and proper treatment:
- Elevated, red lesions of skin: Includes silvery scales. Plaques are characteristic of psoriasis. They are often of varied size and distribution, from small localized patches to big, widespread ones.
- Itching, burning, or soreness: Perioral or around lesions. They can be very debilitating, affecting quality of life and causing discomfort and sleep interference.
- Dry, cracked skin: Can be itchy or bleed. The high turnover of skin cells interferes with the skin’s natural barrier and results in dryness, cracking, and bleeding.
- Thickened, pitted, or ridged nails: Psoriasis of the nails involves the fingernails and toenails and results in nail texture and appearance changes.
- Swollen and stiff joints: Psoriatic arthritis, an inflammatory arthritis that is linked to psoriasis, may lead to swelling, stiffness, and pain in the joints.
Psoriasis signs at the early stages
In the early stages, psoriasis is very mild. Therefore, early psoriasis signs are as follows:
- Small red bumps: possibly on scalp, elbows, or knees.
- Mild Itching: localized.
- Dull, flaky skin: like dandruff or eczema.
- Changes in nails: Pitting or thickening of nails.
4. Psoriasis Causes
The causes of psoriasis are still unknown to researchers worldwide, but mostly they are believed to be a combination of heredity and other triggering external factors.
- Immune System: Fundamentally, psoriasis is an autoimmune disease wherein the T-cells mistake healthy skin cells as foreign and attack them as if they were invaders. A bit of injury is done this way, and inflammation is brought on that accelerates skin cell growth.
- Genetics: If the family member had psoriasis, there was a very high chance for subsequent generations to have the disease. So, it was obvious that the heredity factor was vital. Some genes that were known to be involved in immune regulation have been associated with the condition. But one should know that the mere presence of these genes does not always mean that psoriasis manifests. External triggers are often necessary to activate the disease.
Triggers: The following can initiate or worsen psoriasis flare-ups:
- Stress: Emotional stress can aggravate symptoms of psoriasis to an entirely different level. The relation between stress and developing the disease is a little more complicated; apparently these stress hormones have an effect on the immune function.
- Infections: From all potential infections, streptococcal throat and pyodermas due to bacteria can really act as a triggering mechanism of psoriasis. The immune response to infection sometimes cross-reacts with skin cells.
- Scratches and Cuts: Cuts, scrapes, sunburns, bug bites, and other injuries may also initiate the Koebner phenomenon: psoriasis appearing at the site of injury. This shows the tendency of any skin with a propensity toward psoriasis to trauma.
- A Few Drugs: Beta-blockers, lithium, and antimalarial drugs have been shown to trigger it in some susceptible individuals. It is important for the doctor to know about these medicines because of the family history of psoriasis.
- Weather: Cold, dry weather increases dry skin and sets off inflammation that can worsen the psoriasis flare.
- Drinking and Smoking: They worsen the condition because of high levels of inflammatory levels and suppress immune function. Subsequently, they may hinder psoriasis therapy effectiveness.
5. Psoriasis Treatment: Finding Relief & Managing Symptoms
- Psoriasis treatments aim to slow skin cell growth and remove scales. Options include steroidal creams and ointments (topical therapy), light therapy (phototherapy), and oral or injected medications. The treatment depends on the severity of the psoriasis and the patient’s response to previous treatments. Some commonly recommended treatments include corticosteroids, vitamin D analogues, retinoids, calcineurin inhibitors, salicylic acid shampoos and scalp solutions, coal tar, and anthralin.
- Topical therapy includes corticosteroids, vitamin D analogues, retinoids, calcineurin inhibitors, salicylic acid shampoos and scalp solutions, coal tar, and anthralin, as discussed above. These treatments can be used alone or in combination with other treatments, but may require repeated treatments.
- Light therapy is a first-line treatment for moderate to severe psoriasis, involving controlled exposure to natural or artificial light. Light therapy, such as UVB and PUVA phototherapy, slows skin cell growth. Systemic medications like methotrexate, cyclosporine, and biologics target specific immune system parts. Oral medications like Apremilast reduce inflammation.
Psoriasis treatments have significantly advanced, with the introduction of biologics, biosimilars, and newer treatments too, as discussed below:
- Biologics: Biologics are targeted therapies directed at elements in the immune system that contribute to psoriasis by blocking cytokines related to inflammation. Biologics include TNF-alpha inhibitors, IL-17 inhibitors, IL-23 inhibitors, and IL-12/23 inhibitors; these agents’ main mechanism of action is to block inflammation-related proteins.
- Biosimilars: Biosimilars, which are highly similar to reference biologics, offer potentially lower-cost alternatives and undergo rigorous testing to ensure efficacy and safety. They can also increase access to biologic therapies for more patients, thereby enhancing overall healthcare.
6. How to Cure Psoriasis Permanently: The Quest for a Cure
At this moment, psoriasis is incurable. Yet, investigations continue into novel therapies and a possible cure. People with psoriasis can gain symptomatic long-term relief and good quality of life through possibly successful continuous management treatment.
7. Psoriasis Prevention
Diet doesn’t necessarily cause psoriasis, but some foods may affect flare-ups. One has to focus on the foods to prevent psoriasis flare-ups:
- Anti-Inflammatory Diet: Prioritize fruits, vegetables, whole grains, and healthy fats.
- Omega-3 Fatty Acids: In fish, flaxseed, and walnuts, potentially will decrease inflammation.
- Reduce Processed Foods, Red Meat, and Dairy: These worsen inflammation.
- Discover Food Sensitivities: Monitor potential culprits with a food diary.
- Achieve Healthy Weight: Obesity can aggravate psoriasis.
Living with Psoriasis: Daily Life Tips
- Moisturize Often: Keep the skin hydrated to avoid dryness and cracking.
- Avoid Triggers: Determine and avoid as much as possible exposure to triggers.
- Manage Stress: Use relaxation methods such as yoga or meditation.
- Seek Support: Join support groups or online forums.
- Comply with Treatment Plans: Follow prescribed drugs and therapies.
- Live a Healthy Lifestyle: Exercise, have a balanced diet, and ensure good sleep.
Psoriasis might be a trying experience, yet through appropriate handling and an active approach, one may effectively manage their symptoms and have a successful life. Be sure to seek professional consultation with a dermatologist so one can design an individualized treatment program and take care of concerns.
8. When to Book an Appointment with Your Doctor
Book an appointment with your doctor:
- If you suspect that you are having psoriasis.
- If your symptoms are so severe that they intrude upon or affect your daily life.
- If there is pain or swelling in any of your joints.
- If you are experiencing side effects from the psoriasis treatment.
9. Conclusion
Psoriasis is one of those chronic conditions that an individual can live well with effective management. Identify the triggers, follow a strict therapy regimen, and engage in a healthy lifestyle; those are the three most important points to consider for minimizing flare-ups and improving the quality of life. Professional advice from a dermatologist is necessary for patient-centered optimal results.
Yashoda Hospitals offers comprehensive psoriasis care, combining advanced medical expertise with a patient-centered approach. Our dermatologists are skilled in diagnosing and treating all types of psoriasis, providing access to a wide range of therapies, including topical treatments, phototherapy, and systemic medications. We are dedicated to empowering patients with the knowledge and resources needed to manage their condition and achieve clearer, healthier skin.
Have any questions or concerns about your health? We’re here to help! Call us at +918929967127 for expert advice and support.












 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

