Gastroparesis Demystified: Navigating Symptoms, Causes, and Advanced Treatment

Gastroparesis is a disorder that causes mild or inefficient contractions of the stomach muscles, slowing food movement through the small intestine. This slow digestion can result in uncomfortable symptoms. Measures that are effective in managing the disease prove utmost importance in enhancing the standard of quality of living, preventing malnutrition, and managing related complications.
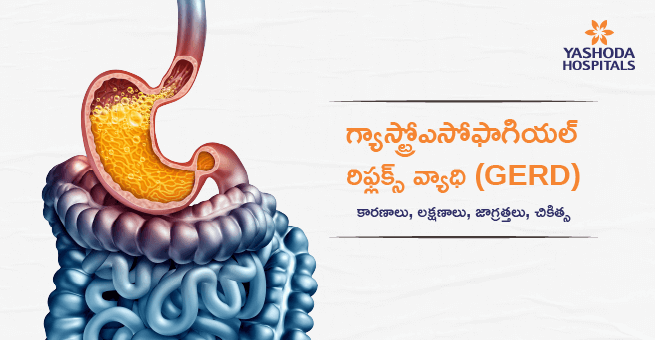
What is Gastroparesis?
Gastroparesis, also known as delayed gastric emptying, is a disorder associated with slowing or cessation of movement of food from the stomach to the small intestine, although it does not present a blockage in the stomach or intestines. The muscles usually contract to pass on food through the digestive tract. However, this gastroparesis slows down or doesn’t work at all in the stomach’s movement. This condition prevents the stomach from being efficiently emptied. While its exact cause remains unclear, it is sometimes linked to diabetes. In some cases, it can develop after surgery or a viral illness.
Gastroparesis is difficult to differentiate from other disorders like functional dyspepsia due to the overlap of upper gastrointestinal symptoms. Thus, a confirmed diagnosis of gastroparesis requires measurement of stomach emptying time via an appropriate test, such as gastric scintigraphy or breath testing. Several novel pharmacologic agents and interventions are in the pipeline and may eventually help tailor individualized therapy for patients with gastroparesis.
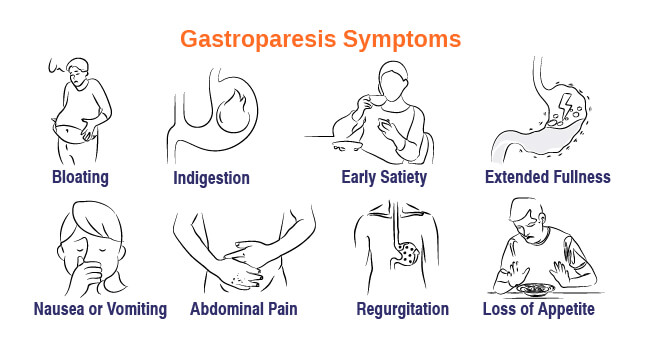
Gastroparesis Symptoms
Some of the common symptoms of gastroparesis include:
- Bloating: The sensation of being bloated or swelling.
- Indigestion: Feeling discomfort in the upper abdomen.
- Early satiety: Getting filled too early while eating.
- Extended fullness: The state of staying too long to get fully satiated with food.
- Nausea and vomiting: Sick feelings or wanting to throw up.
- Pain in the upper abdomen: This can be pain or ache in the stomach region.
- Regurgitation: Undigested food vomiting out.
- Loss of appetite: Interest in eating goes down.
- Acid reflux/heartburn: Sharp, burning sensations in the chest or throat.
- Constipation: Difficulty in defecating.
- Blood sugar variability: Difficult to manage steady blood sugars.
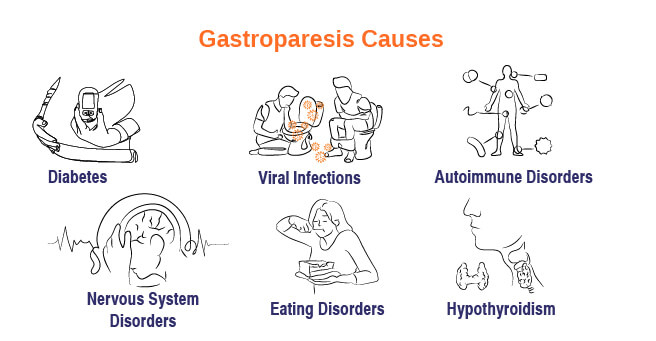
Gastroparesis Causes
The exact cause of the gastroparesis is not known. However, gastroparesis can be caused by damage to the vagus nerve, which controls stomach muscles and manages the digestive tract. A damaged vagus nerve may cause food to stay in the stomach longer. Some of the specific causes include:
- Diabetes: High blood sugar in diabetes usually causes nerve damage over time, disrupting the stomach contractions.
- Surgery: Surgery on the stomach or its adjacent organs like the esophagus or intestines can, at times, destroy the nerves controlling stomach emptying. Viral Infections: Certain viral infections affect the nerves governing stomach functions.
- Viral Infections: In some cases, certain viral infections will affect the nerves controlling the functioning of the stomach.
- Autoimmune Disorders: Autoimmune disorders such as systemic lupus erythematosus and scleroderma can cause muscle and nerve damage in the GI tract.
- Medications: Pain relievers, antidepressants, and anticholinergic drugs, for example, are known to slow stomach emptying.
- Nervous System Disorders: Nervous system disorders such as Parkinson’s disease and multiple sclerosis might also damage nerves that regulate digestive system functions.
- Eating Disorders: Conditions such as anorexia and bulimia affect the digestive system’s normal functions.
- Hypothyroidism: This is an underactive thyroid gland, slowing down bodily functions, including digestion.
Gastroparesis Complications
Gastroparesis can lead to the following complications if left untreated or not treated promptly:
- Nutritional Deficiencies: The failure to digest and absorb nutrients appropriately because of slow stomach emptying leads to malnutrition. This may present as weight loss, vitamin deficiencies, and general weakness.
- Dehydration: Repeated vomiting and an inability to hold fluids may result in dehydration. Symptoms of dehydration include thirst, dizziness, weakness, and low urine output. In severe cases, dehydration can require hospitalization and fluid replacement therapy.
- Weight Loss: Nausea, vomiting, and early satiety, combined with inadequate nutrient absorption, can lead to significant weight loss, which will further affect overall health and well-being.
- Complications of Acid Reflux: Gastroparesis causes the stomach to bulge, creating a pathway from the stomach’s top to escape stomach acid into the esophagus. Chronic acid reflux can bring about complications that the esophagus may endure, such as heartburn and inflammation (esophagitis).
- Blood Sugar Complications: Gastroparesis disrupts the normal, regulated movement of food through the digestive system. This can also disrupt the normal, regulated delivery of glucose into the bloodstream. When food lingers for too long in the stomach, the blood sugar may become too low. When food finally moves on, the blood sugar may surge. These changes are particularly difficult for people with diabetes, and they can exacerbate gastroparesis.
- Bezoar and Gastric Outlet Compaction: A bezoar is a mass of compacted, hardened food that becomes lodged in the stomach. It develops from parts left behind during stomach emptying. A bezoar may grow too large to pass through the outlet at the bottom of the stomach. It can obstruct the outlet and make it difficult for any other food to pass. Healthcare providers treat bezoars with medication to dissolve them, or if necessary, surgery to remove them.
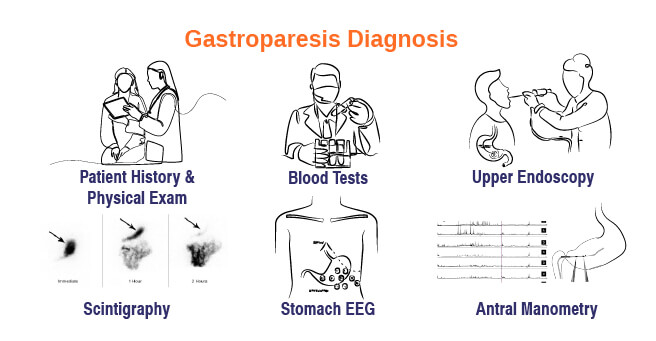
Gastroparesis Diagnosis
Diagnosing the gastroparesis involves the following diagnostic tests:
Medical History Evaluation and Physical Examination
- The medical history will be taken in depth, such as the symptoms, medical conditions, medications, and family history. A physical examination will be carried out to identify signs of dehydration, malnutrition, and other complications.
Blood Tests
- Checking for underlying causes like diabetes, anemia, and electrolyte imbalances and also assessing the liver and kidney functions by performing the blood tests.
Imaging Tests
- Upper endoscopy: A flexible tube with a camera on its end is inserted through the mouth to view the esophagus and stomach.
- Scintigraphy (gastric emptying studies): The primary test used to diagnose gastroparesis is called a gastric emptying study, also known as scintigraphy. This involves eating a small meal containing harmless radioactive material. A scanner then tracks how quickly the food empties from your stomach, revealing any delays in gastric emptying time.
Other Tests
- EEG of the stomach: Electrical activity of the stomach muscles.
- Antral manometry: This measures the force of stomach muscle contractions.
Gastroparesis Treatment
Medications
- Prokinetics: These are the medications that stimulate gastrointestinal motility and are the first-line treatment for gastroparesis. They stimulate muscle contractions in the stomach and can also help relieve nausea.
- Motilin Agonists: These medications mimic the effects of motilin by activating the same receptors in the digestive tract.
- Serotonin Agonists: These medications are prescribed to improve constipation but haven’t been fully evaluated for gastroparesis treatment.
- Dopamine Antagonists: They block dopamine and improve gastric motility and nausea.
Gastric Therapies
- Gastric Electrical Stimulation (GES): Implantation of a device to stimulate stomach contractions.
- Botox Injections: Injection of botulinum toxin into the pyloric sphincter to relax muscle and improve stomach emptying.
Surgery
This is the final resort in gastroparesis treatment, modifying the stomach to facilitate food passage. Procedures include:
- Pyloroplasty: Modifies the pylorus, the muscular valve at the bottom of the stomach, to allow food to empty out.
- Gastric Bypass Surgery: A partial gastrectomy removing or closing off part of the stomach and creating a new outlet from the stomach to the small intestine.
Dietary Modifications & Lifestyle Modifications
Dietary Changes
- Small & Frequent Meals: Take 5-6 small meals in a day instead of three large meals to reduce the pressure on the stomach.
- Low-Fat Diet: Avoid high-fat foods such as fried foods, greasy foods, and fatty meats.
- Decreased Fiber: Reduce the consumption of high-fiber foods like whole grains, beans, and some fruits and vegetables because they are hard to digest.
- Liquid or Pureed Foods: Add liquids, soups, and pureed foods to the diet when tolerated.
- Avoid Trigger Foods: Identify what foods make symptoms worse, such as carbonated drinks, alcohol, and caffeine.
Lifestyle Changes
- Stress Management: Engage in stress-reducing techniques like yoga, meditation, or deep breathing exercises since stress is known to aggravate gastroparesis.
- Regular Exercise: Engage in regular physical activity, such as walking or light exercise, after meals to aid digestion. Avoid strenuous exercise immediately after eating.
- Healthy Weight: Weight loss can improve gastroparesis symptoms and overall health in overweight or obese individuals.
- Smoking Cessation: Smoking can worsen digestive problems and should be avoided.
When to Seek Apointment?
One should see the doctor if:
- Persistent or worsening symptoms: For example, if the symptoms of nausea and vomiting, or abdominal pain or early satiety don’t improve after changing what one eats and drinks.
- Unexplained weight loss: In case one’s losing weight so drastically without another apparent cause for it.
- Dehydration: If one is feeling dehydrated, experiencing dizziness, fatigue, or having a decreased urination rate.
- Severe vomiting: If one is vomiting repeatedly or if the vomiting is severe and has some other worrisome signs.
- Blood in the vomit: If one sees any blood in the vomit.
Conclusion
Gastroparesis significantly affects a person’s quality of life, but there are various management strategies that may be adopted by an individual with gastroparesis to better live with the condition and enhance his or her well-being. A patient suffering from gastroparesis may manage symptoms with proper diet changes, lifestyle adjustments, and active involvement with gastroenterologists.
Yashoda Hospitals is one of the most well-known healthcare providers that specializes in digestive health. The gastroenterologists there are experienced and provide patients with gastroparesis comprehensive care, including advanced diagnostic procedures, personalized treatment plans, and support to help them manage their condition effectively.
Have any questions or concerns about your health? We’re here to help! Call us at +918929967127 for expert advice and support.









 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More

