Frequently asked questions about COVID-19 (SARS Cov2)

At a Glance:
4. What is community spread of COVID-19?
5. Can COVID-19 spread through food, pets, packages, mosquitoes?
6. How can a person protect themself and their family from COVID-19?
8. Are face masks effective in protecting against COVID-19?
9. How does COVID-19 affect children?
10. How does COVID-19 affect pregnant women?
11. Who are at higher risk of getting a serious infection with COVID-19?
12. What is incubation period?
13. What are the signs and symptoms of COVID-19?
14. What if a person comes in contact with a suspected case of COVID-19?
15. Are there any home-based tests for COVID-19?
16. Who should get tested for COVID-19?
18. Is there a treatment available for COVID-19?
What is coronavirus?
Coronavirus is a type of virus that is known to cause certain infections within the respiratory tract of human beings ranging from the common cold to more severe conditions like Severe Acute Respiratory Syndrome (SARS).
Viruses are microscopic organisms that are invisible to the naked eye and even smaller than bacteria. They are made up of genetic material i.e the RNA or DNA surrounded by a protein coat.
Viruses are incapable of surviving and reproducing on their own. Viruses replicate inside the cells of other organisms, thereby causing certain infectious diseases.
What is COVID-19?
Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) or COVID-19 (Coronavirus Disease 2019) is an acute respiratory and infectious disease. COVID-19 is an outbreak that began in December 2019 caused by the spread of new type of coronavirus started in Wuhan, China. The disease has now spread in many countries across the world, so it is termed as a pandemic.
How does COVID-19 spread?
It is believed that the first infections of COVID-19 in human beings were associated with a live animal market. However, now the virus is spreading from person-to-person.
The main way of spread is due to close contact with affected persons. The infection gets transmitted from one person to another through respiratory droplets that may be produced when an infected person coughs or sneezes, which may land in the nose or the mouth of the unaffected person.
The coronaviruses have poor survivability on inanimate surfaces over days or weeks. However, COVID-19 can get transmitted if an unaffected person touches the surface of an object that might be recently contaminated with the droplets holding the virus. Subsequent touching of one’s mouth, eyes or nose can lead to the spread of the virus.
Can virus stay in air?
Infections of the respirator tract can be transmitted from one person to another through droplets. These droplets maybe of different sizes. For the purpose of their ability to spread infection they may be categorised as:
- Droplet particles >5-10 μm in diameter are referred to as respiratory droplets
- Droplet particles <5μm in diameter are referred to as droplet nuclei
As per the available data evidence, COVID-19 virus gets transmitted from one person to other through respiratory droplets and contact with contaminated surfaces.
Airborne transmission of COVID-19 has not been reported.
Droplet transmission takes place when a person is in in within 1 m close contact with a person with respiratory symptoms like coughing or sneezing. The virus can reach the body through the mucous membrane within the eyes, mouth and nose when exposed to potentially infective respiratory droplets of the person who is sneezing.
Alternately, transmission can also take place indirectly through fomites or contamination of the surfaces around the infected person.
Airborne transmission on the other hand is different from droplet transmission as occurs due the presence of microbes within droplet nuclei. Since droplet nuclei are particles <5μm in diameter, they tend to remain in the air for a longer duration and get transmitted to others over longer distances beyond 1 m.
Airborne transmission in COVID-19 can be suspected only in specific circumstances of medical procedures or support treatments where aerosols are generated like suctioning, nebulization, non-invasive positive-pressure ventilation etc.
What is community spread of COVID-19?
In the initial stages, the infection was primarily acquired by individuals who had a history of travel to affected geographical locations.
Community spread, on the other hand, indicates the presence of the infection in an area where individuals may not necessarily have a history of travel and who are not sure how or where they became infected.
COVID-19 infection has been seen to be spreading easily and sustainably in the community in certain affected geographic areas.
Can COVID-19 spread through food, pets, packages, mosquitoes?
As stated earlier, coronaviruses generally spread from person-to-person through respiratory droplets. There is no sufficient evidence to prove that COVID-19 transmission could be directly associated with food. However, it is always a good practice to wash hands with soap and water for at least 20 seconds before preparing or eating food for safety from foodborne infections, known or unknown.
Coronavirus may be surviving on the food items purchased such as fresh vegetables, fruits, meat. It is recommended to enjoy the fresh products after thorough cleaning and proper cooking.
Even though the infection seems to have initially been transmitted from wild animals, there is not enough data that shows that pets or domesticated animals might become a source of infection with this new coronavirus. Since certain other types of diseases can get transmitted from animals to people, it is always recommended that good hygiene practices like washing hands be followed when dealing with pets.
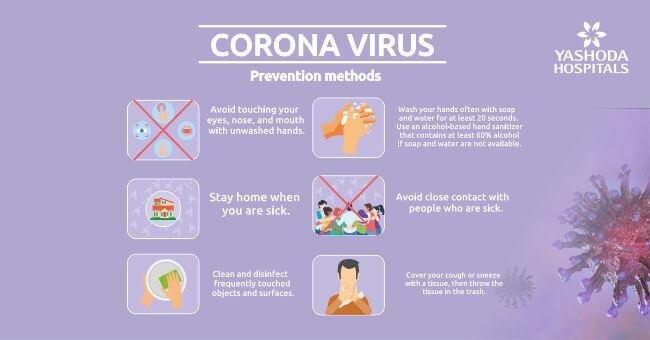
How can a person protect themself and their family from COVID-19?
Simple preventive actions practiced every day can help in reducing the risk of getting sick with COVID-19. Such measures hold even greater importance for persons having chronic medical conditions and the elderly. Some of these measures are:
- Social distancing and avoiding close contact with people who are sick or suspected to be sick.
- Persons who are sick should stay at home except to get medical care.
- Persons having cough and sneezing should sneeze in the elbow or use disposable tissues that should be carefully disposed after use.

- Hands should be washed often with soap and water for at least 20 seconds. Hand washing is extremely important before eating or preparing food, after nose-blowing, coughing, sneezing, or using the toilet. Hands should always be washed with soap and water if they are visibly dirty.
- Alcohol-based hand sanitizer with at least 60% alcohol is recommended in case of non-availability of soap and water.
- Surfaces and objects that are frequently touched should be regularly cleaned and disinfected. E.g. tabletops, mobile phones, keypads of computers and laptops, light switches, doorknobs, doorbells, and cabinet handles, etc.
Do’s and Don’ts
Do’s
- Hand washing should be done often with soap and water or alcohol-based sanitizers. Hand should be washed even if they appear to be clean.
- A handkerchief/tissue should be used to cover the nose and mouth while sneezing and coughing. If using a handkerchief, it should be washed thoroughly with soap and water. Disposable tissues should be thrown into closed bins immediately after use.
- Sneezing if possible should be done in the elbow.
- If a person is experiencing fever, difficulty in breathing and cough, a doctor should be consulted. One must cover the nose and mouth with a mask/cloth if visiting the doctor. Always follow the guidance of the physician.
- Avoid participating in gatherings of large number of people
- Maintain adequate distance from someone who is coughing, sneezing. At least 2 metres apart should be sufficient.
- A person who is caring for someone with flu like symptoms, like cough and a fever he/she should use a face mask to cover the nose and mouth for personal protection.
- Frequently touched surfaces such as doorknobs, doorbell buttons, handles,car doors, elevator buttons etc. should be cleaned and disinfected with regular household disinfectant or soap and water frequetly.
Don’ts
- As the hands come in contact with many inanimate surfaces, it is advisable to avoid touching the eyes, nose and mouth. The virus can get transferred from the contaminated surface to eyes and nose through the hands.
- A person should avoid having a close contact with anyone, if he/she is experiencing cough and fever
- One must avoid spitting in public, more so if he/she is having symptoms
- A person having symptoms of COVID-19 should not self-medicate
- Avoid travel or going out of the house if a person has flu-like symptoms, except for seeking medical attention if required.
What is social distancing?
As defined by the Ministry of Health and Family Welfare, “Social distancing is a non-pharmaceutical infection prevention and control intervention implemented to avoid/decrease contact between infected person from others to stop or slow down the rate and extent of disease transmission in a community.”
Are face masks effective in protecting against COVID-19?
Using surgical face masks by an infected person can help in reducing the risk of infecting other people. However, there is no enough evidence to prove that wearing a face mask can effectively prevent a person from being infected with the virus. Personnel protective equipment (PPE) like masks is generally recommended as a preventive measure for persons who are at a high risk of exposure to infectious agents like healthcare professionals, sanitary workers, and patient caregivers at home.
As advised by the World Health Organization (WHO), healthy individuals should be using a mask only when:
- They are required to care for a person with suspected COVID-19
- They have suspected symptoms such as coughing or sneezing
Mask is used in combination with frequent hand hygiene using soap and water or an alcohol-based sanitizer.
Those using a mask must know how to use it and dispose it properly.
How does COVID-19 affect children?
As per the available data, it is seen that children are affected less frequently and the symptoms are relatively minor. However, it is recommended not to be complacent with children’s health. Social distancing and hand hygiene should be adhered for prevention against the disease, especially if the child has some underlying disease like asthma.
How does COVID-19 affect pregnant women?
As per the available data and evidence, the illness among pregnant women after COVID-19 is not any severe or different from a non-pregnant adult. Further, there is no evidence that there could be a negative effect on the fetus of a pregnant woman or transmission from mother to baby during COVID-19 infection. Pregnant women should follow regular handwashing and avoid getting in direct contact with suspected infected persons. In case of any symptoms self-isolation should be followed under the guidance of a doctor.
Who are at higher risk of getting a serious infection with COVID-19?
While anyone can become infected with the virus, it is seen that persons with certain underlying medical conditions like diabetes, hypertension, cardiovascular disease, cancer and chronic respiratory diseases like asthma or chronic obstructive pulmonary disease are prone to developing severe symptoms and complications. Similarly, elderly persons are also at a high risk of severe infection.
What is incubation period?
Incubation period is the period between exposure to the virus and onset of symptoms of the condition. The incubation period for COVID-19 is observed to be between 2-14 days.
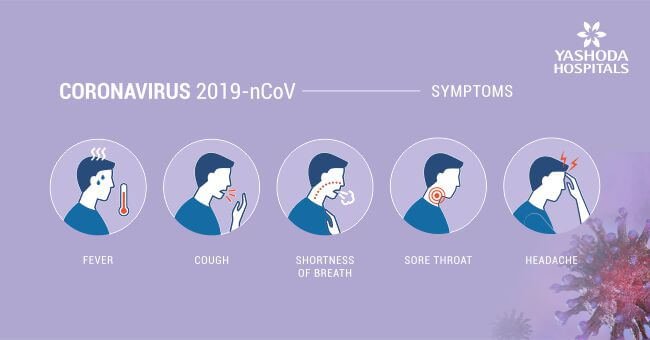
What are the signs and symptoms of COVID-19?
The most common symptoms of COVID-19 documented so far are flu-like symptoms such as:
- Dry cough and sore throat
- Difficulty in breathing
- Fever
- Muscle pain or body ache
- Tiredness or fatigue
Pneumonia, sepsis, acute respiratory distress syndrome, and septic shock is seen in severe cases, often leading to death.
What if a person comes in contact with a suspected case of COVID-19?
Ideally, it is recommended to stay at least one meter away from symptomatic persons of COVID-19 to reduce the risk of infection through respiratory droplets.
It is important that a person who has come in contact with a suspected case to avoid touching own face with unwashed hands. This is so because the virus enters the body via the eyes, nose and/or mouth.
Immediately after contact, the first thing that should be done is to wash hands with soap and water for at least 20 seconds. If soap and water are not available, cleaning the hands with alcohol-based solutions or gel is recommended.
Individuals who develop symptoms like fever, cough, difficulty breathing, muscle pain or tiredness after coming in contact with a COVID-19 confirmed/suspected case should contact a healthcare service provider preferably by telephone or online consultation if available or visit their nearest healthcare facility with due precautions. Also, maintain self isolation as recommended by the WHO guidelines.
The consulting physician would decide based on medical history whether a laboratory test for the virus is needed or not. If a person must undergo further testing, the procedure to follow and advise where and how the test can be performed will be explained by the consulting physician.
Are there any home-based tests for COVID-19?
There are no scientifically evidenced, FDA approved tests available for home-based testing of COVID-19.
Who should get tested for COVID-19?
Ministry of Health and Family Welfare, Government of India recommends testing for
Symptomatic persons who:
- Have a history of travel in the last 14 days
- Were/are in close contact with a confirmed case. A confirmed case is a person with laboratory confirmation of COVID-19 infection, irrespective of clinical signs and symptoms.
- Are healthcare staff
- Are hospitalized persons with conditions like Influenza Like Illness (ILI) or Severe Acute Respiratory Illness (SARI) or severe pneumonia.
Asymptomatic direct and high-risk contacts of persons with confirmed COVID-19 should be tested once between day 5 and day 14 of coming in contact with the affected person. Direct and high-risk contact include:
- Persons residing in the same household as the confirmed case
- Healthcare workers who came in contact with the infected person during an examination without adequate protection as per the recommendation of the WHO.
The advice on testing of specific subgroups within the population may vary depending on the stage of the outbreak and the geographical location of a person’s residence. Factors that are being taken into consideration by authorities across different countries include:
- Level of community transmission of COVID-19
- Resource ability to test
- Availability of necessary equipment for testing
- Any locally relevant criteria
What is quarantine?
Quarantine is a preventive measure to control the possible spread of the disease by separating a person or group of people who have been exposed to the infection but have yet not developed the symptoms of infection, from others who have not been exposed.
Quarantining is usually done for the incubation period of the infection. In the case of COVID-19, it is 14 days from the last date of exposure. 14 days is the longest incubation period recorded for similar coronaviruses.
A person who has uneventfully completed 14 days of quarantine for COVID-19 is not considered to be a risk for spreading the virus to others due to that exposure.
Is there a treatment available for COVID-19?
There is no definitive treatment for the disease at present. Clinical management is focused on the management of symptoms like fever and breathing difficulties. Supportive care with oxygen therapy, fluid management, etc has been seen to be effective for hospitalized persons with COVID-19.
At the moment, there is no approved antiviral therapy for the treatment of COVID-19. Treatment is primarily management of symptoms. A person who has been affected with COVID-19 and who presents with mild symptoms, may be recommended recovery by staying at home by the treating physician.
Monitoring of the symptoms and isolation is advised to prevent possible infection of the other family members. Follow up with physician through a telephonic consult if possible is advisable.
When recovering at home, it is strongly recommended that a person should not self-medicate.
Self-care for symptomatic management can be done by:
- Adequate rest and sleep
- Keeping warm
- Maintaining sufficient hydration by drinking plenty of liquids
- Depending on the need, a person may use a room humidifier or take a hot shower or gargle to help ease a sore throat and cough
Medications for management of COVID-19
The World Health Organization does not recommend self-medication with any medicines, including antibiotics, as a prevention or cure for COVID-19. However, depending on the severity of symptoms, a physician may prescribe certain medications only for the management of symptoms like:
- Pain relievers
- Cough syrup or medication for sore throat
- Antibiotics work only on bacterial infections. Since COVID-19 is caused by a virus, antibiotics are not prescribed as a means of treatment of COVID-19. Antibiotics should only be used if prescribed by a physician to treat an associated bacterial infection.
The Indian council of Medical Research has released an advisory on the use of hydroxy chloroquine for use as a prophylactic agent solely for high risk population that includes:
- Asymptomatic healthcare workers involved in care of COVID-19 cases
- Asymptomatic caregivers of laboratory confirmed cases COVID-19.
This medication should be used only on prescription of an authorized medical practitioner due to the high risk of adverse reactions, and should not be used to get a false sense of security. This medication doesn’t replace the need of social distancing and other preventive precautions
Are there any vaccines for COVID-19?
Currently, there are no vaccines to prevent human coronaviruses, including that of COVID-19. Some pharmaceutical companies are developing candidates for vaccination. However, the process of any drug development is long, which takes months or sometimes years. Extensive testing to determine the product’s safety and efficacy are needed before it can be used on a large scale.
Consequently, prevention of the COVID-19 infection by social distancing assumes a greater role in preventing further spread of the virus.
Where can I get more information on COVID-19?
There are many resources available on the internet that are disseminating information on COVID-19. However it is recommended that a person looking for information on the disease and related aspects should refer to the resources of government bodies including the Ministry of Health and Family Welfare, Government of India, World Health Organization, European Centre for Disease Prevention and Control, Centre for Disease Control to name a few, or acclaimed healthcare and research institutes and hospitals. Some of the recommended resources are:
- The Indian Council of Medical Research (ICMR), New Delhi, Testing Laboratories, https://covid.icmr.org.in/index.php/testing-facilities
- Ministry of Health and Family Welfare, Government of India, COVID-19 Updates, https://www.mohfw.gov.in/
- World Health Organization, Homecare for patients with COVID-19 presenting with mild symptoms and management of their contacts, https://www.who.int/publications-detail/home-care-for-patients-with-suspected-novel-coronavirus-(ncov)-infection-presenting-with-mild-symptoms-and-management-of-contacts
- Government of India, Important Information For Corona – Virus: https://www.mygov.in/covid-19
- Ministry of Health and Family Welfare, Government of India COVID-19 testing – when and how? https://www.mohfw.gov.in/pdf/FINAL_14_03_2020_ENg.pdf
- World Health Organization, Coronavirus disease (COVID-19) advice for the public: When and how to use masks https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks
- European Centre for Disease Prevention and Control; Q & A on COVID-19 https://www.ecdc.europa.eu/en/novel-coronavirus-china/questions-answers
About Author –













 Appointment
Appointment WhatsApp
WhatsApp Call
Call More
More